Bulimia Nervosa Symptom Checker for Men
This confidential tool helps you understand if you might be experiencing symptoms of bulimia nervosa. It's designed specifically for men and focuses on symptoms often overlooked in male patients. The results are not a diagnosis but can guide you toward appropriate next steps.
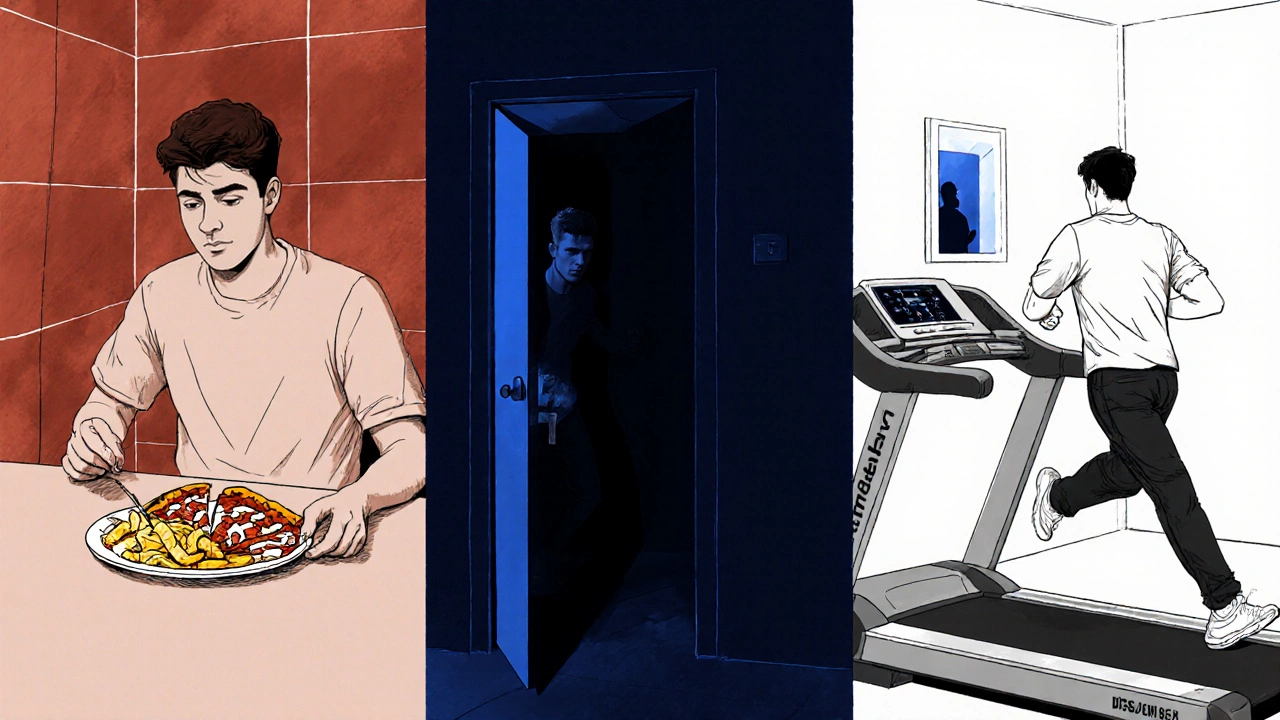
When we talk about Bulimia Nervosa - a serious eating disorder marked by binge‑eating episodes followed by compensatory actions like self‑induced vomiting, excessive exercise, or laxative abuse, most people picture a young woman. That picture is a myth. In reality, bulimia nervosa in men is a hidden but growing health concern, and the stigma that it’s “only a women’s problem” keeps many guys from getting help.
Key Takeaways
- Bulimia affects roughly 1‑2% of men, yet most diagnoses are still women‑centric.
- Symptoms in men often include secretive bingeing, frequent bathroom trips after meals, and unusual weight‑loss methods such as over‑exercise.
- Diagnosis follows the same DSM‑5 criteria used for women, but clinicians must look for male‑specific cues.
- Effective treatment combines Cognitive Behavioral Therapy, nutritional counseling, and, when needed, medication.
- Breaking the stigma starts with open conversation, education, and supportive networks.
What Is Bulimia Nervosa?
According to the DSM‑5, bulimia is defined by three core features: recurrent binge‑eating episodes, inappropriate compensatory behaviors, and self‑evaluation that is overly influenced by body shape and weight. Binge episodes involve eating an objectively large amount of food in a short period while feeling a loss of control. Compensation can be vomiting, misuse of laxatives or diuretics, fasting, or compulsive exercise.
While the diagnostic checklist doesn’t differentiate by gender, the lived experience can vary. Men often feel pressure to hide their struggles due to cultural expectations around masculinity, which leads to a more secretive pattern of behavior.
How Bulimia Shows Up in Men
Male presentations sometimes diverge from the classic textbook case. Typical signs include:
- Frequent trips to the bathroom after meals, especially if the individual is trying to conceal vomiting.
- Excessive focus on muscle definition rather than thinness; many men aim for a “lean, ripped” look.
- Unexplained electrolyte imbalances, dental erosion, or sore throat that a doctor attributes to acid reflux but actually stem from repeated vomiting.
- Unusual weight‑loss tactics like extreme cardio sessions, sauna use, or excessive protein‑shake consumption to offset binge calories.
Psychologically, men may report intense guilt, shame, and a belief that seeking help would make them look weak. The internal dialogue often centers on performance-both in the gym and in life-making it harder to admit a problem that feels “unmanly.”
Why the Myth Persists
The idea that eating disorders are a women‑only issue is reinforced by media, research, and even some health‑care settings. Popular TV shows and magazines rarely feature male sufferers, and surveys historically oversampled women. This creates a feedback loop: clinicians expect women, women are diagnosed more, and the data keeps showing a gender gap.
Stigma also plays a huge role. In many cultures, men are taught to “tough it out,” and any admission of vulnerability is labeled as a weakness. That cultural script makes men less likely to talk about body image concerns, even though the pressure to look a certain way is just as strong.
Prevalence and Statistics
Recent studies from 2023‑2024 indicate that about 1.1% of adult men in the U.S. meet criteria for bulimia, compared with 1.6% of women. In Australia, a 2022 national survey found 0.7% of men reported binge‑purge cycles in the past year, a figure that likely underestimates the true prevalence because of under‑reporting.
Age‑wise, men in their late teens to early thirties are most affected, mirroring patterns seen in women. However, a smaller but notable group of older men (40‑60) also experience bulimic behaviours, often linked to life stressors like divorce, job loss, or retirement.
Diagnosis Process
Diagnosing bulimia in men follows the same systematic approach used for women, but clinicians should be attuned to male‑specific cues. The process typically includes:
- Clinical interview focusing on eating habits, body image, and compensatory behaviours.
- Physical exam checking for signs such as enamel erosion, swollen salivary glands, and callused knuckles (Russell’s sign).
- Laboratory tests for electrolyte disturbances, especially potassium and chloride, which can be life‑threatening if ignored.
- Psychological assessment to gauge co‑occurring conditions like depression, anxiety, or substance use.
Because men often hide their purging, a thorough medical history is essential. Asking open‑ended questions like, “Do you ever feel you’ve lost control over how much you eat?” can uncover binge episodes that the patient might not volunteer.
Effective Treatment Options
Evidence‑based treatment for bulimia doesn’t change with gender. The gold standard remains Cognitive Behavioral Therapy (CBT), which targets distorted thoughts about food and body image and teaches healthier coping skills.
Complementary interventions that work well for men include:
- Nutritional counseling: A registered dietitian can develop a balanced meal plan that reduces binge urges and supports muscle maintenance.
- Medication: Selective serotonin reuptake inhibitors (SSRIs), especially fluoxetine, have shown efficacy in reducing binge‑purge cycles.
- Exercise guidance: Instead of unrestricted workouts, men benefit from structured, moderate‑intensity programs that prevent compulsive over‑training.
- Support groups: Male‑specific or mixed groups where participants share experiences can lower feelings of isolation.
Family involvement is also powerful. When a partner or close friend learns how to respond non‑judgmentally, the individual feels safer seeking help.
Supporting a Male Loved One
If someone you care about shows signs of bulimia, consider these steps:
- Approach the conversation with empathy: “I’ve noticed you’ve seemed stressed about food lately-do you want to talk about it?”
- Avoid blame: Focus on health concerns rather than appearance.
- Encourage professional help: Offer to research therapists who specialize in eating disorders.
- Educate yourself: Understanding that bulimia is a medical condition, not a lack of willpower, changes how you react.
- Be patient: Recovery is a marathon, not a sprint. Celebrate small victories, like a week without purging.

Breaking the Stigma
Changing the narrative starts with visibility. Sharing personal stories, promoting male‑focused awareness campaigns, and incorporating men into research designs all send the message that bulimia is not gender‑exclusive.
On a community level, workplaces and gyms can host mental‑health workshops that specifically address eating‑disorder myths. Schools should include balanced education on body image that features both male and female role models.
Resources and Next Steps
If you suspect you or someone you know is dealing with bulimia, these resources can help:
- National Eating Disorders Association (NEDA) helpline - 1‑800‑931‑2237 (US) / 1800‑100‑247 (Australia)
- ANAD (Australia) - 1800 555 787 - offers free telephone counseling.
- Online support forums such as r/EatingDisorders with active male participants.
- Find a therapist on the Academy of Nutrition and Dietetics directory who lists “Eating‑Disorder Specialist”.
Taking the first step-whether it’s a phone call, a web search, or a conversation with a trusted friend-can change the trajectory of a life that feels stuck in a secret cycle.
Quick Comparison of Major Eating Disorders
| Feature | Bulimia Nervosa | Anorexia Nervosa | Binge‑Eating Disorder |
|---|---|---|---|
| Core Behaviour | Binge + compensatory actions (vomiting, laxatives, excessive exercise) | Severe restriction + intense fear of weight gain | Recurrent binge episodes without regular compensatory actions |
| Typical Body Weight | Usually normal or slightly above normal | Often significantly underweight | Often normal or overweight |
| Gender Ratio | ~1:1 male‑female (still under‑diagnosed in men) | ~10:1 female‑male | ~2:1 female‑male |
| Medical Risks | Electrolyte imbalance, esophageal tears, dental erosion | Bone loss, heart complications, organ failure | Type‑2 diabetes, hypertension, cardiovascular disease |
| First‑Line Treatment | CBT‑E (CBT for eating disorders) + nutrition counseling | Family‑based therapy, CBT, medical stabilization | CBT, weight‑management programs, sometimes medication |
Frequently Asked Questions
Can men really develop bulimia?
Yes. Studies from the past five years show that roughly 1‑2% of adult men meet the diagnostic criteria for bulimia, but many go undetected because of stigma and lack of gender‑specific screening.
What are the physical signs to watch for?
Frequent bathroom trips after meals, swollen salivary glands, enamel erosion, chronic sore throat, and unexplained electrolyte disturbances are common red flags.
Is treatment for men different from women?
The core therapies-CBT‑E, nutritional counseling, and SSRIs-are the same for both sexes. However, incorporating discussions around masculinity, body‑image pressures specific to men, and tailored exercise plans improves engagement.
How can I support a male friend with bulimia?
Approach with empathy, avoid blame, encourage professional help, and educate yourself about the condition. Offer to attend appointments or look up male‑focused support groups together.
Where can I find professional help?
Search for therapists listed as “Eating‑Disorder Specialist” on accredited directories, call national helplines like NEDA (1‑800‑931‑2237) or Australia’s ANAD (1800‑555‑787), and consider joining male‑friendly support forums.


Comments
William Nonnemacher
Bulimia in men is real and you can't brush it off as a women's issue. The data shows men are affected too. Ignoring it just keeps the stigma alive. You need to look at the facts not the stereotypes. Stop pretending it's not happening.
October 12, 2025 at 05:00
Alex Ramos
This tool is a step forward, but it must be used responsibly; men often hide their struggles, and the medical community needs to take notice! We should promote awareness, disseminate resources, and encourage open dialogue-now more than ever.
October 12, 2025 at 22:13
Edmond Abdou
Hey there, thanks for sharing this tool. It’s great to have something tailored for men, and it can open up conversations that have been missing. If anyone feels uneasy, reaching out to a professional is a solid move 😊. Keep the conversation going.
October 13, 2025 at 16:16
Sydnie Baker
One must acknowledge the pernicious stigmatization that has traditionally relegated eating pathology to a gendered narrative. The epistemological lacuna regarding male bulimia necessitates a paradigmatic shift in both clinical praxis and sociocultural discourse. By integrating neurobehavioral biomarkers and psychodynamic frameworks, we can ameliorate diagnostic fidelity.
October 14, 2025 at 10:20
Benjie Gillam
Yo, think of this like a hidden bug in the system of our minds-yeah, it’s a mess but you can debug it. First, recognize the pattern of binge‑purge cycles, then map out triggers like stress or body image pressure. Therapy, nutrition counseling, and maybe medz can help. It’s a tough road but definatly doable.
October 15, 2025 at 04:23
Naresh Sehgal
Listen up! This checker isn’t just some gimmick-it’s a lifeline! Men hide their struggles, and we need to smash that silence NOW. Grab the results, call a therapist, and start a real conversation. No more playing it safe.
October 15, 2025 at 22:26
Johnny VonGriz
Nice work on the tool. It really gives people a place to start, especially when they’re feeling stuck. If anyone needs extra help, there are groups and professionals out there ready to listen.
October 16, 2025 at 16:30
Real Strategy PR
We must condemn the ignorance that still surrounds male eating disorders.
October 17, 2025 at 10:33
Doug Clayton
That’s a solid point thanks for bringing it up I think more guys will feel seen after this
October 18, 2025 at 04:36
Michelle Zhao
It is utterly scandalous that society continues to relegate bulimia to a feminine domain. The theatricality of denial only deepens the suffering of men who grapple with this silent torment. Let us, with gravitas, dismantle such archaic narratives and usher in an era of inclusive understanding. The stage is set for change.
October 18, 2025 at 22:40
sneha kapuri
Honestly, this whole “men can have bulimia too” narrative feels like a trend chasing political correctness. People just want to expand victimhood labels without real data. It’s a distraction from genuine health issues that need focus.
October 19, 2025 at 16:43
Ash Charles
Don’t let the stigma stop you-take charge, use the checker, and if the risk feels high, get professional help immediately. You’ve got the strength to fight this.
October 20, 2025 at 10:46
debashis chakravarty
One must scrutinize the methodological rigor of such self‑assessment tools; while they serve an introductory purpose, they cannot supplant a comprehensive clinical evaluation. Consequently, patients should be cautioned against overreliance on anecdotal scoring mechanisms.
October 21, 2025 at 04:50
Daniel Brake
I wonder how cultural narratives shape the willingness of men to disclose binge‑purge behaviors, and whether alternative frameworks might reduce that barrier.
October 21, 2025 at 22:53
Emily Stangel
The prevalence of bulimia nervosa among men, though historically underreported, warrants rigorous scholarly attention. Epidemiological studies indicate that up to ten percent of male patients present with binge‑purge patterns comparable to their female counterparts. This parity challenges the entrenched gendered stereotypes that have long dominated clinical textbooks. Consequently, medical curricula must integrate male‑specific case studies to foster diagnostic acumen. Moreover, the psychosocial determinants, including body image pressures within certain subcultures, amplify vulnerability. Researchers have identified a correlation between participation in competitive sports and heightened disordered eating symptoms among men. It is imperative that treatment modalities be tailored, recognizing that men may experience distinct shame dynamics. Cognitive‑behavioral therapy, when adapted to address masculine norms, demonstrates promising outcomes. Pharmacotherapy, as an adjunct, should be considered with careful monitoring of side‑effects uniquely reported by male patients. Family involvement, although beneficial, often encounters resistance due to societal expectations of stoicism. Healthcare providers must therefore employ empathetic communication strategies to mitigate avoidance. Public health campaigns should depict diverse body types and explicitly include male narratives to reduce stigma. Accessibility to qualified professionals remains uneven, underscoring the need for telehealth expansion. Finally, continuous community education, supported by organizations such as NEDA, can facilitate early detection and intervention. In sum, a comprehensive, gender‑inclusive approach is essential to ameliorate the burden of bulimia nervosa among men.
October 22, 2025 at 16:56