Perceived Exertion Calculator
Understand Your Exercise Intensity
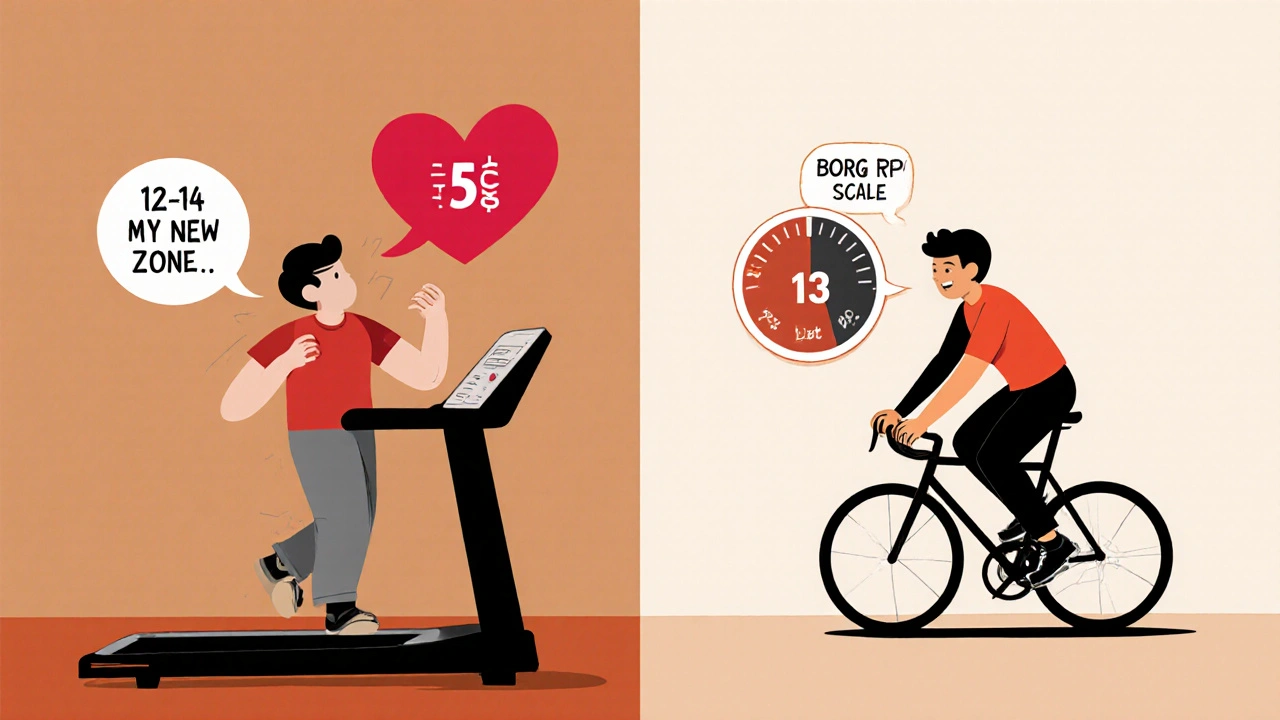
Beta-blockers reduce your heart rate response, making traditional heart rate monitoring unreliable. Use the Borg Rating of Perceived Exertion (RPE) scale to find your safe exercise zone.
How Intensity Works on Beta-Blockers
On beta-blockers, aim for RPE 12-14 where you can talk comfortably but not sing.
Find Your Safe Zone
Tell us about your experience level:
Feeling worn out during a walk or struggle to keep up on the treadmill isn’t just because you’re out of shape. If you’re taking beta-blockers for high blood pressure, heart rhythm issues, or heart failure, your body’s natural response to exercise has been turned down - on purpose. These medications slow your heart rate so your heart doesn’t have to work as hard. But that same effect makes it harder for your body to get the oxygen it needs when you move. The result? Fatigue that feels out of proportion to your effort. You’re not lazy. You’re not failing. Your meds are just changing the rules.
Why Beta-Blockers Make Exercise Feel Harder
Beta-blockers like metoprolol, propranolol, and atenolol block adrenaline from hitting your heart. That’s good for your heart - it reduces strain and lowers blood pressure. But it also means your heart can’t speed up the way it used to when you start moving. Studies show these drugs can cut your maximum heart rate by 20-30%. So if you used to hit 170 bpm on a run, you might now max out at 120-130 bpm, even if you’re pushing just as hard.
This isn’t just about feeling tired. Your heart’s ability to pump blood drops by 15-20% during hard exercise. That means less oxygen reaches your muscles. Your VO₂ max - the gold standard for aerobic fitness - typically falls by 10-15% on beta-blockers. You’re not losing muscle strength, but your body’s ability to use oxygen during activity is limited. That’s why you might feel winded walking uphill or struggle to finish a 5K that used to feel easy.
How Other Medications Compare
Not all heart meds slow you down the same way. ACE inhibitors like lisinopril or calcium channel blockers like amlodipine rarely affect heart rate during exercise. Diuretics might make you dehydrated or cramp, but they don’t cap your heart rate. Beta-blockers are unique in directly limiting how fast your heart can beat during activity. That’s why the old rule - “aim for 70% of your max heart rate” - doesn’t work anymore. If your heart rate is artificially held low, chasing a number can lead to overexertion, dizziness, or worse.
Stop Tracking Heart Rate. Start Listening to Your Body.
The biggest mistake people make? Trying to hit their old heart rate targets. That’s not just useless - it’s dangerous. Instead, shift to methods that measure how hard you feel you’re working, not how fast your heart is beating.
The talk test is the simplest and most reliable. If you can talk comfortably but not sing, you’re in the right zone. If you can’t say a full sentence without gasping, you’re going too hard. If you’re chatting like you’re on a coffee date, you can probably push a little more. This method works because it matches your body’s real oxygen needs, not a number on a watch.
The Borg Rating of Perceived Exertion (RPE) scale gives you a bit more precision. It runs from 6 (no effort at all) to 20 (maximum effort). For most people on beta-blockers, aiming for 12-14 (light to moderate effort) is safe and effective. That’s where you feel like you’re working, but not struggling. If you used to train at RPE 17, you might now need to stay at 14-15. Don’t fight it. Adjust.
How to Modify Your Workouts
Don’t quit exercise - just change how you do it. Here’s what works:
- Extend your warm-up. Go from 5-10 minutes to 10-15. Let your heart and lungs adjust slowly. Jumping into a brisk walk or light bike ride right away can shock your system.
- Lengthen your sessions. Since you’re working at lower intensity, you need more time to get the same benefit. Aim for 180-188 minutes of moderate activity per week instead of the standard 150. That’s about 30-40 minutes, 5-6 days a week.
- Choose low-impact, steady movement. Walking, cycling on flat ground, swimming, and elliptical training are great. Avoid sudden bursts or high-intensity intervals unless you’re under supervision.
- Modify strength training. Beta-blockers don’t weaken your muscles, so you can still lift. But reduce the weight by 15-20% and keep the reps the same. Focus on control, not max effort. Two sets of 12-15 reps with lighter weights beats one heavy set that leaves you breathless.
- Hydrate before, during, and after. Some people on beta-blockers notice they don’t sweat as much - even when they’re warm. That’s a red flag. Dry mouth and no sweat during mild activity mean your body can’t cool itself properly. Drink water even if you’re not thirsty.
What to Watch Out For
Exercise is safe - but not if you ignore warning signs. Stop and sit down if you experience:
- Resting heart rate below 45 bpm with dizziness or lightheadedness
- Systolic blood pressure dropping below 90 mmHg during activity
- Chest pain, pressure, or tightness that doesn’t go away with rest
- Severe shortness of breath that doesn’t improve after stopping
- Unusual fatigue that lasts more than 24 hours after exercise
If any of these happen, contact your doctor. These aren’t normal side effects - they’re signals your body needs a different plan.
Real People, Real Adjustments
On Reddit’s beta-blocker community, one user wrote: “On 100mg metoprolol, my 5K time went from 25:30 to 29:15 - but I feel better now because I stopped chasing my old pace.” Another shared: “Switching to the talk test let me walk 45 minutes every day without passing out.” These aren’t exceptions. They’re the rule.
People on propranolol report higher fatigue rates (78%) than those on metoprolol (63%), but the fix is the same: stop measuring heart rate, start measuring effort. The goal isn’t to return to your pre-med self. It’s to find a new version of yourself - one that moves safely, consistently, and without fear.
The Future Is Personalized
Doctors are starting to use cardiopulmonary exercise testing (CPET) to design custom exercise plans for people on beta-blockers. This test measures exactly how your body uses oxygen during activity, so your program is tailored to your limits - not a generic guideline.
Wearables are catching up too. Apple Watch’s latest software now includes beta-blocker-adjusted heart rate zones. But don’t rely on them yet. Clinical validation is still pending. Your body’s signals - how you feel, how you breathe, how you talk - are still the most accurate tools you have.
Keep Moving. Just Differently.
Exercise isn’t optional when you’re on beta-blockers - it’s essential. It helps your heart stay strong, your blood pressure stable, and your energy levels higher over time. But you have to play by the new rules. Forget the numbers. Listen to your breath. Notice your effort. Adjust your pace. Extend your time. Protect your body. You’re not broken. You’re adapting. And that’s how you stay healthy - not by fighting your meds, but by working with them.

Comments
mona gabriel
Been on metoprolol for 8 years. Stopped chasing heart rate numbers and started walking like I’m sipping tea instead of racing a train. Best decision ever. No more dizzy spells. Just steady movement. My dog approves.
November 18, 2025 at 09:39
Phillip Gerringer
You’re all missing the point. Beta-blockers are a Band-Aid on a broken cardiovascular system. If you’re relying on exercise to compensate for poor lifestyle choices, you’re just delaying the inevitable. The real issue is metabolic syndrome. Fix your diet first. No amount of walking fixes insulin resistance.
November 18, 2025 at 15:42
Matt Webster
Phillip, I hear you. But for a lot of us, diet’s already been fixed. We’re eating clean, sleeping well, reducing stress. The meds are just part of the equation. The goal isn’t to be a triathlete again-it’s to walk the dog without needing a nap afterward. That’s victory.
November 20, 2025 at 01:26
Jaylen Baker
YES. Exactly. I used to think I was failing because my heart rate wouldn’t climb. Then I learned RPE. 12-14. That’s my new 17. I walk 40 minutes every morning now. No watch. Just breath. And I feel stronger than I have in years. You’re not broken-you’re recalibrated.
November 20, 2025 at 09:50
Nagamani Thaviti
Why do people still think walking is exercise its like breathing and you think you are doing something great
November 22, 2025 at 05:13
Merlin Maria
While the talk test is empirically sound, it lacks the granularity of a properly calibrated CPET protocol. Without objective VO₂ kinetics, you’re navigating by candlelight in a cathedral of physiological complexity. Your anecdotal ‘feeling’ is not data-it’s heuristic noise.
November 23, 2025 at 05:28
Sharmita Datta
They say beta blockers are for heart but i think they are for control the population if you move too fast your heart rate spikes and then they say oh you need more meds and you become dependent and they sell you more pills and the system wins
November 24, 2025 at 02:57
Fiona Hoxhaj
How quaint. The notion that one can ‘listen to one’s body’ implies a Cartesian unity between mind and physiology that has been thoroughly debunked in modern neurocardiology. Your body is a biomechanical system under pharmacological modulation-your ‘feelings’ are epiphenomena, not guides. Relying on subjective metrics is a form of epistemic laziness.
November 25, 2025 at 02:39
Daniel McKnight
Man, I used to think I was weak because I couldn’t run like before. Then I found out my heart rate cap was the drug, not me. Now I lift light, walk slow, and still feel like I’m doing something real. No guilt. No shame. Just movement. That’s the win.
November 25, 2025 at 09:06
Kamal Virk
The article is well-researched, but it fails to address the psychological toll of being labeled ‘fatigued’ by the medical establishment. We are not broken. We are adapted. And adaptation is not weakness-it is resilience encoded in biology.
November 26, 2025 at 00:07
jeff melvin
Stop glorifying walking. If you’re not sweating and your HR is under 130, you’re not training-you’re strolling. This isn’t wellness, it’s surrender. If you can’t hit 70% of your pre-med max, maybe you should be on a different med
November 27, 2025 at 23:20
Stephen Wark
I’ve been on propranolol for 12 years and I still run marathons. You just need to be tougher. This whole ‘listen to your body’ crap is for people who don’t want to push through. I’ve passed out twice on the track. Still ran the next day. You’re not sick-you’re soft.
November 28, 2025 at 19:01