Reading your prescription label shouldn’t feel like solving a puzzle. Yet, millions of people misunderstand when and how often to take their meds-leading to missed doses, overdoses, or worse. A 2023 study found that 41.3% of adults have been confused by their medication timing instructions. That’s not just inconvenient. It’s dangerous.
What Do Terms Like 'Twice Daily' Really Mean?
You’ve seen it: "Take 1 tablet twice daily." It sounds simple. But what does "twice daily" actually mean? Many people assume it means morning and night. Others take both pills at once. Some even space them out every 12 hours without realizing it matters. The FDA now recommends clear, explicit timing: "Take 1 tablet in the morning and 1 tablet in the evening." Why? Because "twice daily" is too vague. A 2021 trial at Massachusetts General Hospital showed patients who got exact times were 34.7% more likely to take their meds correctly. That’s not a small difference-it’s the difference between your blood pressure staying under control or spiking dangerously. Even terms like "once daily" can be misleading. Some people think "once daily" means anytime they remember. But for drugs like levothyroxine (used for thyroid issues), taking it with food or coffee can block absorption entirely. The label should say: "Take on an empty stomach, at least 30 minutes before breakfast."Why "As Needed" Is the Most Dangerous Phrase on a Label
"Take as needed for pain" sounds flexible. But without a maximum daily dose, it’s a recipe for overdose. A 2023 Consumer Reports survey found that 67.8% of people didn’t know the safe limit for painkillers labeled "as needed." For example, acetaminophen (Tylenol) has a maximum daily dose of 3,000-4,000 mg, depending on liver health. But if your label just says "take as needed," you might not realize that two 500 mg pills every 6 hours adds up to 4,000 mg in 24 hours. That’s the limit. Taking more can cause liver failure. Always look for the phrase: "Do not exceed [X] tablets in 24 hours." If it’s not there, ask your pharmacist. Don’t guess.Units Matter: mL Is Not a Teaspoon
Liquid medications are especially risky. A 2021 NIH study found that 63.8% of pharmacy labels still used "teaspoon" or "tablespoon"-even though those aren’t precise measurements. A household teaspoon can hold anywhere from 3 to 7 mL. A standard medicine cup? Often inaccurate. The FDA and U.S. Pharmacopeia now require all liquid prescriptions to use milliliters (mL). If your label says "take 5 tsp," that’s outdated and unsafe. It should say "take 25 mL." Always use the dosing cup or syringe that comes with the bottle-not a kitchen spoon. A 2022 study showed that using kitchen spoons led to a 27.4% error rate in dosing.Abbreviations Like B.I.D. and T.I.D. Are Out
You might see "b.i.d." or "t.i.d." on your label. Those are Latin abbreviations for "twice daily" and "three times daily." But here’s the problem: only 37.4% of patients understand them, according to the American Medical Association. The AMA and FDA both recommend avoiding these entirely. Instead, labels should spell it out: "Take two times a day" or "Take three times a day." If you see "b.i.d.", ask your pharmacist to rewrite it in plain language. You have the right to understand your meds.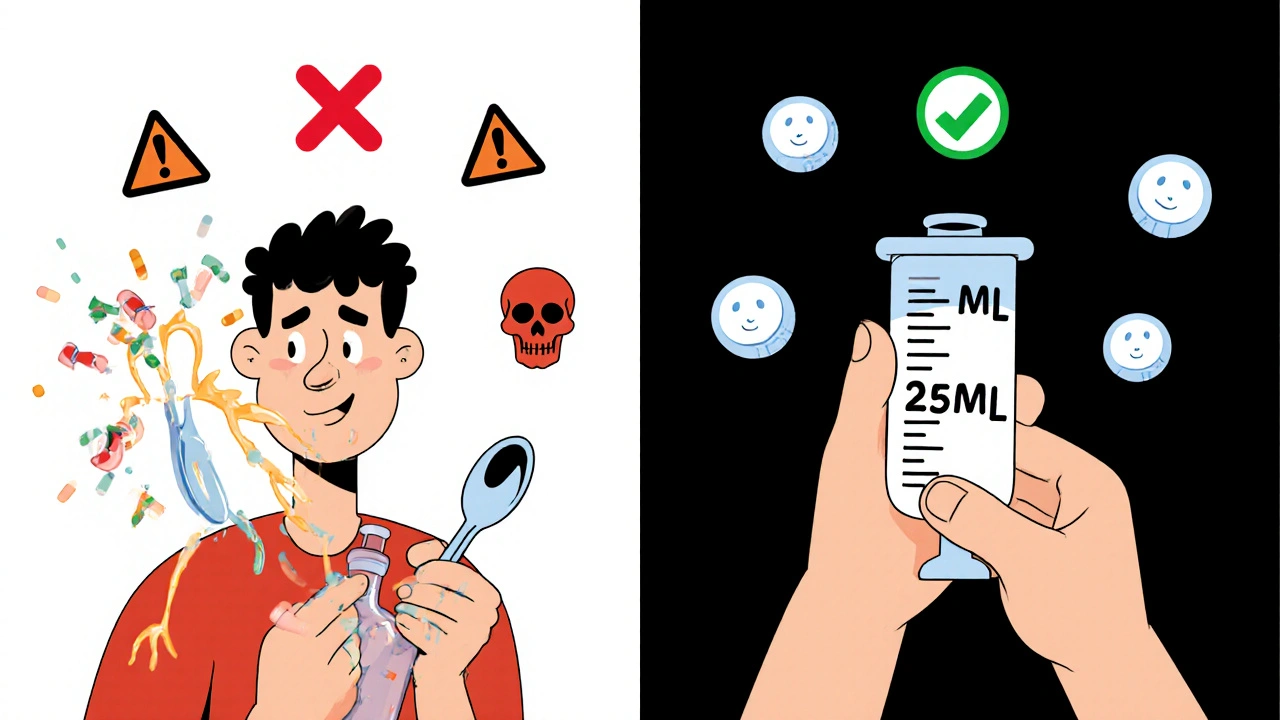
Timing Isn’t Just About Morning and Night
For some drugs, the exact hour matters. Cancer meds, insulin, and certain heart medications have narrow therapeutic windows. The FDA’s Oncology Center of Excellence now requires labels to say things like: "Take between 8:00 AM and 10:00 AM." Why? Because if you take it at 6 AM one day and 8 PM the next, your body doesn’t get consistent levels. That can make the drug less effective-or even toxic. Even for non-cancer drugs, timing affects side effects. Metformin, used for diabetes, causes stomach upset if taken on an empty stomach. Labels that say "Take with breakfast and dinner" help patients avoid nausea. One patient on PatientsLikeMe reported that switching from "take two tablets daily" to "take one with breakfast and one with dinner" cut their stomach issues in half.Shift Workers and Irregular Schedules: What Now?
What if you work nights? Or your schedule changes every week? "Take in the morning and evening" doesn’t work if you sleep during the day. Dr. Michael Wolf’s 2022 study found that 22.3% of night-shift workers misinterpreted "morning" and "evening" instructions. The solution? Ask your pharmacist for a personalized schedule. You might get: "Take 1 tablet when you wake up and 1 tablet 12 hours later." Pharmacists are trained to adjust timing for your lifestyle. Don’t assume the label is set in stone. Bring up your work hours, sleep schedule, or meal times. They can help you reframe the instructions so they fit your life.What to Do If Your Label Is Still Vague
Despite FDA rules, many pharmacies still use outdated language. A 2023 study found that 82.7% of retail pharmacy labels still used vague terms like "twice daily." CVS got it right in 93% of cases. Walgreens? Only 38%. Independent pharmacies? Just 28%. If your label says "as directed," "b.i.d.", or "take with meals" without specifying when, don’t accept it. Ask your pharmacist:- "What time should I take this?"
- "Is there a maximum number I can take in a day?"
- "Should I take it with food or on an empty stomach?"
- "Can you write it out in plain words?"

Technology Is Changing Labels-For the Better
New tools are making this easier. Starting in 2024, the FDA began testing augmented reality labels. Scan your pill bottle with your phone, and a video shows you exactly when to take your medicine-complete with a clock and visual cues. Also, a new standardized "Medication Schedule Grid" is coming by 2027. It’ll show a weekly chart with boxes for each dose. No more guessing. But you don’t have to wait. Use free apps like Medisafe or MyTherapy. They let you input your prescription and send you reminders with exact times. Sync them with your phone calendar. Set two alarms if you need to.When to Call Your Doctor or Pharmacist
Don’t wait until you feel sick. Call if:- You’re unsure when to take your medicine
- Your schedule changed (new job, travel, shift work)
- You missed a dose and don’t know what to do
- The label conflicts with what your doctor told you
Final Checklist: What to Look For on Every Prescription Label
Before you leave the pharmacy, check your label against this list:- Is the dose in milliliters (mL) for liquids? (Not teaspoons)
- Does it say exact times? (e.g., "with breakfast" and "with dinner")
- Is there a maximum daily dose for "as needed" meds?
- Are Latin abbreviations like "b.i.d." or "t.i.d." absent?
- Does it say whether to take it with or without food?
- Is there a phone number to call if you’re confused?
What does "twice daily" mean on a prescription label?
"Twice daily" means two doses in one day, but it doesn’t specify when. The FDA now recommends saying "Take one tablet in the morning and one tablet in the evening" to avoid confusion. Many people mistakenly take both doses at once or space them too far apart. Exact timing improves safety and effectiveness.
Can I use a kitchen spoon to measure liquid medicine?
No. A kitchen teaspoon holds between 3 and 7 milliliters-far from the standard 5 mL used in medicine. Using one can lead to under- or overdosing. Always use the dosing cup or syringe that comes with your prescription. The FDA requires all liquid medications to list doses in milliliters (mL), not teaspoons.
What should I do if my prescription says "as needed" without a daily limit?
Ask your pharmacist for the maximum daily dose. For example, acetaminophen (Tylenol) should never exceed 4,000 mg per day. Without this limit, you risk liver damage. If the label doesn’t include it, request a corrected label or a written note from your prescriber.
Why do some labels say "take with food" and others say "take on an empty stomach"?
Some medicines work better or cause fewer side effects based on whether your stomach is full or empty. For example, levothyroxine must be taken on an empty stomach because food blocks absorption. Others, like metformin, cause stomach upset unless taken with food. Always follow the label’s direction-never assume.
I work nights. How do I take my medicine if the label says "morning and evening"?
Tell your pharmacist your schedule. They can adjust the timing to fit your routine-for example, "Take one when you wake up and one 12 hours later." The goal is consistent intervals, not matching "morning" and "evening" to the clock. Many patients with irregular shifts benefit from this personalized advice.
Are abbreviations like b.i.d. and t.i.d. still allowed on prescriptions?
They’re not banned, but they’re strongly discouraged. The FDA and American Medical Association recommend spelling out instructions like "twice daily" or "three times daily" because only about 37% of patients understand the abbreviations. If you see them, ask your pharmacist to rewrite the label in plain language.


Comments
Robert Merril
so i took my blood pressure med at 8am and 8pm for 3 years then one day the pharmacist says 'no no no it's morning and evening' and i'm like bro it's the same thing also why is my bottle still saying b.i.d. like it's 1987
November 16, 2025 at 22:04
Roberta Colombin
I appreciate this article. It is important that patients understand their medications. Many elderly individuals are confused by the terminology used on prescription labels. Clear, plain language is a basic right. Thank you for emphasizing this.
November 18, 2025 at 08:52
Dave Feland
The FDA’s ‘recommendations’ are not regulations. The pharmaceutical-industrial complex has no incentive to improve clarity. The real issue? They profit from patient confusion. Look at the 82.7% statistic-this is systemic negligence. And don’t get me started on the AR labels. That’s just surveillance disguised as convenience.
November 19, 2025 at 03:45
Eva Vega
The pharmacokinetic variability introduced by non-standardized dosing intervals significantly compromises therapeutic efficacy and increases the risk of adverse events. The use of milliliters over household measurements is non-negotiable from a clinical safety standpoint. Furthermore, the elimination of Latin abbreviations aligns with evidence-based health literacy initiatives.
November 19, 2025 at 15:13
George Gaitara
I just got my thyroid med and it says 'take on empty stomach' but my pharmacy gave me a cup that says '5 tsp' and I'm like are you kidding me right now? I'm not a toddler I don't use kitchen spoons for medicine also why is my doctor still writing b.i.d. on the script?? i called the pharmacy and they said 'oh that's just how it's printed' like that's acceptable??
November 20, 2025 at 17:07
Abdul Mubeen
They’re putting AR labels on bottles? Who’s coding this? Who’s monitoring the data? This isn’t innovation-it’s a backdoor for Big Pharma to track your compliance. And don’t tell me it’s ‘for your safety.’ They’ve been tracking us for years through insurance claims. This is just the next step.
November 22, 2025 at 02:47
Jennie Zhu
The implementation of standardized medication schedules is a critical advancement in patient-centered care. The integration of milliliter-based dosing and the elimination of ambiguous temporal references significantly mitigate iatrogenic risk. It is imperative that healthcare providers prioritize linguistic accessibility in pharmaceutical communication.
November 22, 2025 at 21:59
Kathy Grant
I used to take my diabetes meds whenever I remembered. Then I started having crazy stomach cramps. One day I asked my pharmacist, 'what if I take them with food?' She looked at me like I'd just solved world hunger. Turns out metformin was wrecking my gut because I was taking it on an empty stomach. Now I take one with breakfast, one with dinner. No more pain. Just… peace. I wish I’d known sooner.
November 24, 2025 at 17:48
Noel Molina Mattinez
why do people care so much about morning and evening when you can just take it when you wake up and 12 hours later like literally everyone on night shift does this already
November 26, 2025 at 00:10
Ashley Unknown
I’ve been taking my blood pressure med for 7 years and I just found out that 'twice daily' means not at the same time?? I thought I was being responsible taking both pills together so I wouldn’t forget. I’ve been doing it wrong this whole time. My husband says I’m dumb. My mom says I’m lucky I didn’t die. My doctor didn’t explain it. The pharmacy didn’t explain it. I just got a label that said 'b.i.d.' and I thought it was a brand name. I feel like I’ve been gaslit by the medical system.
November 26, 2025 at 17:22
Georgia Green
i used to use a kitchen spoon for my kid's antibiotics until one day i realized the cup that came with it had a line at 5ml and my spoon held 7. i almost killed him. never again. always use the syringe. always. i still have nightmares about that.
November 27, 2025 at 21:17
Christina Abellar
Always check the label. Always ask. Always insist on plain language. It’s not being difficult-it’s being smart.
November 28, 2025 at 04:18
Margo Utomo
I used to think 'as needed' meant 'whenever I feel like it' 😅 until my liver started screaming at me. Now I have a sticky note on my fridge: 'MAX 4000MG' 📝💊 and my phone pings me at 8am, 2pm, and 8pm. Life’s better with alarms and emojis. 🙌
November 29, 2025 at 15:14
Matt Wells
The continued use of Latin abbreviations on pharmaceutical labels constitutes a fundamental breach of the duty of care owed to patients. Such terminology is archaic, exclusionary, and demonstrably harmful. The American Medical Association’s position is not merely a recommendation-it is an ethical imperative. Institutions that persist in using 'b.i.d.' or 't.i.d.' are not merely negligent; they are complicit in medical illiteracy.
December 1, 2025 at 09:58