When a patient is prescribed a medication, they expect to get exactly what their doctor ordered. But in hospitals and nursing homes, that’s not always what happens. Behind the scenes, institutional formularies are deciding which drugs get used - and which ones get swapped out, even if the prescription says otherwise. This isn’t about pharmacy errors. It’s a deliberate, regulated system designed to cut costs and improve safety. But it’s also causing confusion, delays, and sometimes, real harm.
What Exactly Is an Institutional Formulary?
An institutional formulary is a living list of approved medications that a hospital or clinic allows its staff to use. It’s not just a catalog. It’s a rulebook. If a doctor prescribes a drug that’s not on the list, the pharmacist can legally replace it with another - one that’s chemically different but expected to work the same way. This is called therapeutic substitution. In Florida, the law (Statute 400.143) defines it clearly: replacing a prescribed drug with another that has the same clinical effect. That means if a patient was supposed to get brand-name Xarelto, the facility might give them apixaban instead - because both are blood thinners, and apixaban is cheaper. This isn’t random. It’s based on evidence, cost, and safety data reviewed by a committee. These formularies aren’t new. Back in the 1800s, pharmacies kept lists of standard remedies. Today, they’re complex systems managed by teams of pharmacists, doctors, and nurses. The goal? Reduce errors, lower costs, and make sure patients get the most effective drugs available. But the system only works if it’s tightly controlled - and that’s where things get messy.Who Decides What Goes on the List?
It’s not the CEO. It’s not the insurance company. It’s a formal committee mandated by law in places like Florida. Every facility with a formulary must have a team that includes:- The medical director
- The director of nursing services
- A certified consultant pharmacist
Therapeutic Substitution: Safety Tool or Hidden Risk?
Proponents say institutional formularies reduce adverse drug events by 15-30%. That’s huge. In long-term care, where patients take five or more medications daily, a single wrong interaction can be fatal. Formularies help prevent that by limiting high-risk combinations and pushing safer, proven alternatives. One nursing home administrator in Tampa told the American Health Care Association in June 2024 that their quarterly reviews uncovered seven dangerous drug interactions they’d never have spotted otherwise. That’s the win. But the flip side? Confusion. A Reddit thread from March 2024 shared a case where a patient was switched from Xarelto to apixaban during a nursing home stay. When they went back to the hospital, they were switched back - without anyone telling the patient or their family. The patient didn’t know why their medication changed twice in a week. They didn’t know what to tell their doctor. They didn’t know if they were supposed to feel different. That’s not just inconvenient. It’s dangerous. Patients with complex conditions - like heart failure, epilepsy, or psychiatric disorders - often need very specific drugs. Even small changes in formulation can affect how the body absorbs them. A 2023 survey by the American Medical Association found that 78% of physicians worry about bureaucratic barriers when trying to get non-formulary drugs for these patients. And patients? They’re often left in the dark. AARP’s Policy Institute pointed out that most residents in long-term care facilities have no idea their meds were swapped. No consent form. No explanation. That’s not just poor communication - it’s a violation of informed consent.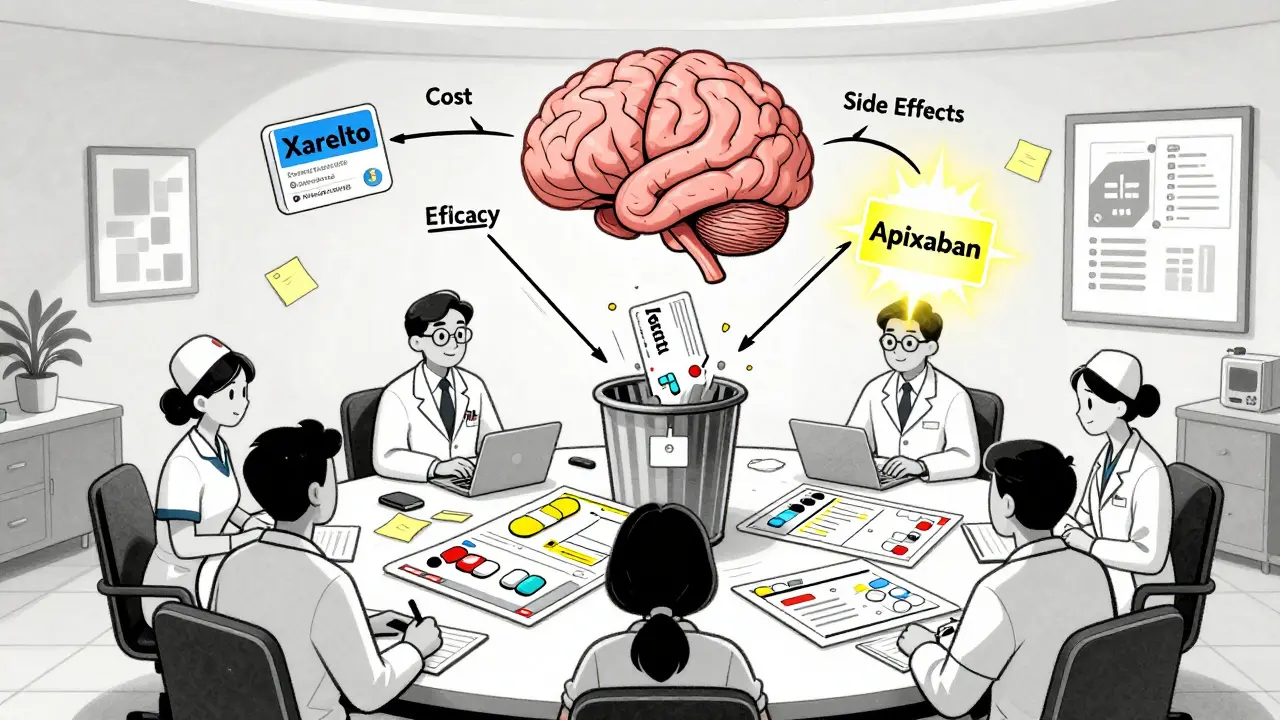
How Formularies Differ from Insurance Plans
People often confuse institutional formularies with insurance formularies. They’re not the same. Insurance formularies control what your plan will pay for. If your drug isn’t on the list, your co-pay jumps. You might need a prior authorization. It’s about cost-sharing. Institutional formularies are about what the hospital can legally give you - even if your doctor wrote a different prescription. It’s not about your insurance. It’s about the facility’s rules. A drug can be covered by your plan but still be banned in the hospital’s formulary. This creates a double layer of control. You might have the right drug on your insurance list, but the hospital refuses to give it because it’s not on their formulary. And if you’re admitted unexpectedly - say, after a fall - you’re stuck with what they’ve got. That’s why many patients end up with inconsistent regimens. They get one drug at the hospital, another at rehab, and a third at home. No one coordinates. No one tracks. And the patient pays the price.Implementation Challenges in Real Hospitals
Setting up a formulary sounds simple. But in practice, it’s a nightmare of paperwork, tech glitches, and training. Florida’s law requires facilities to create written policies within 90 days of launching a formulary. That includes guidelines for substitutions, staff training, and quarterly reviews. Sounds manageable? Think again. A 2024 survey by the Florida Agency for Health Care Administration found that 68% of hospitals had trouble integrating their formulary rules into their electronic health record (EHR) systems. The software didn’t know when to flag a substitution. It didn’t auto-alert nurses. It didn’t log why a drug was changed. Nursing staff, who administer most meds, needed the most training. Many had never heard of therapeutic substitution before. They thought they were just following orders - not making clinical decisions. On average, staff spend 20-30 hours per quarter just updating records, attending meetings, and documenting substitutions. That’s time taken away from patient care. And the tools? They’re not great. Most hospitals rely on outdated templates and manual logs. The American Society of Health-System Pharmacists updated their guidelines in April 2024, recommending bi-monthly - not quarterly - reviews. But few facilities can keep up.Where the System Is Working - and Where It’s Falling Apart
Institutional formularies shine in long-term care. Nursing homes have stable populations. Patients stay for months or years. Medication routines are predictable. That’s why 94% of nursing homes in the U.S. use formal formularies - compared to just 78% of acute care hospitals. In nursing homes, substitutions can prevent falls, reduce delirium, and cut ER visits. The data supports it. But in emergency rooms, ICUs, or surgical units? Things change fast. A patient’s condition can shift in hours. A drug that’s safe today might be dangerous tomorrow. Rigid formularies can delay critical treatment. One ICU nurse in Atlanta told a colleague, “We had to wait two hours for a formulary exception to give a patient epinephrine because it wasn’t on the list. They were crashing. We didn’t have time for paperwork.” The system wasn’t built for emergencies. It was built for consistency. That’s its strength - and its flaw.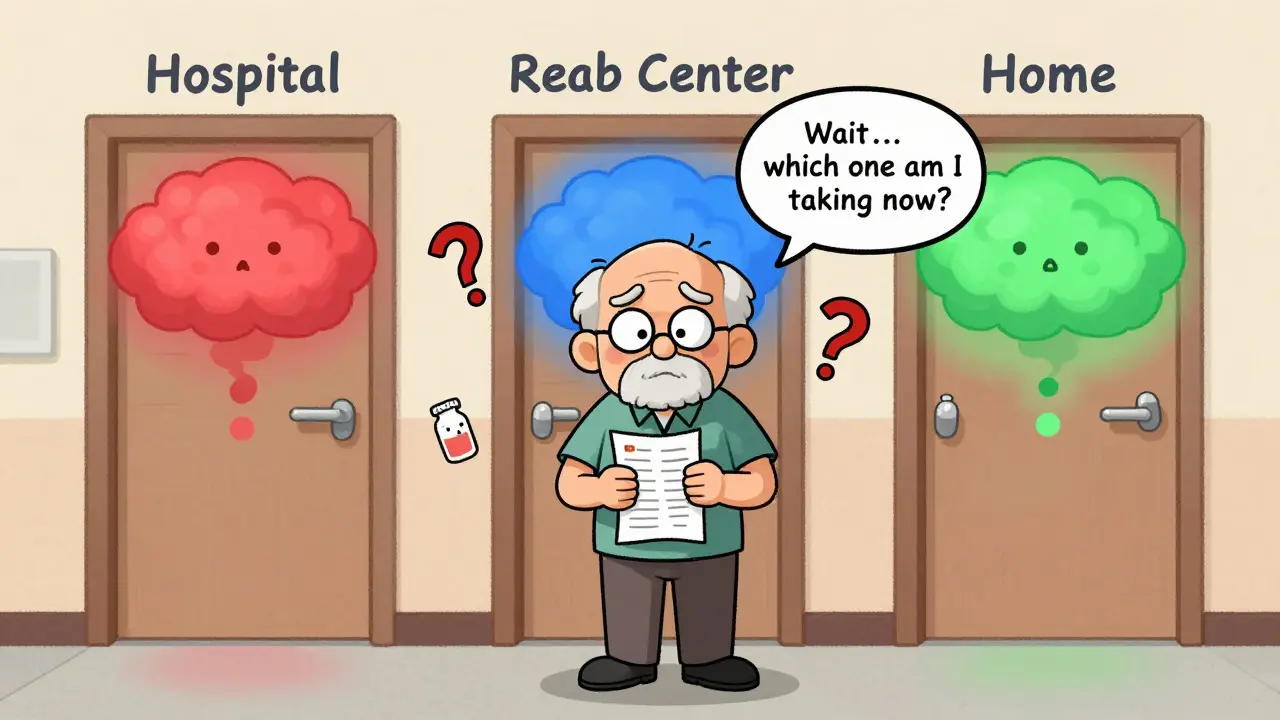
What’s Changing in 2025 and Beyond
The rules are evolving. Florida’s Statute 400.143 was updated on January 1, 2025, to require more detailed monitoring of substitution outcomes. The Centers for Medicare & Medicaid Services (CMS) announced in March 2024 that formulary compliance will now be part of Nursing Home Compare ratings - starting in Q3 2025. That means hospitals with poor substitution tracking could lose funding. The FDA is launching a pilot program in 2025 to standardize how drugs are labeled as “therapeutically equivalent.” Right now, that determination is messy. One drug might be deemed interchangeable in one state, not in another. Standardization could make substitutions safer and more predictable. Looking ahead, AI is coming. Gartner predicts that by 2026, 80% of healthcare systems will use AI-driven formulary tools that adjust in real time based on patient outcomes. Imagine a system that knows a patient had a bad reaction to a substitution last month - and automatically blocks that swap for them in the future. Some hospitals are already testing pharmacogenomics - using a patient’s DNA to guide drug choices. If your genes make you a poor metabolizer of a certain drug, the system could automatically skip it, even if it’s on the formulary. The future isn’t about limiting choices. It’s about personalizing them.What Patients and Families Should Know
If you or a loved one is in a hospital or nursing home:- Ask: “Is this the exact medication my doctor prescribed?”
- Ask: “Was this changed? Why?”
- Ask: “Can I get a copy of the facility’s formulary list?”
- Write down every drug change - name, dose, reason.
- Bring your own medication list to every appointment.
- Don’t assume the pharmacy or nurse knows your full history.
Final Thoughts
Institutional formularies are a necessary tool in a broken system. They help control costs and prevent errors. But they’re not perfect. They were designed for stability, not speed. For consistency, not complexity. And they often ignore the human side of care. The best formularies aren’t the strictest. They’re the most transparent. The ones that involve patients in the conversation. The ones that let doctors override them when needed. The ones that update fast enough to keep up with real medicine. Until then, patients and families need to be their own advocates. Because no algorithm, no committee, and no law can replace a well-informed person asking the right questions.What is therapeutic substitution in a hospital setting?
Therapeutic substitution is when a hospital or clinic replaces a prescribed drug with a different one that’s expected to have the same clinical effect. For example, switching from brand-name Xarelto to apixaban, both blood thinners. This is allowed under institutional formulary rules, as long as it’s documented and approved by the facility’s pharmacy committee.
Are hospitals required to have a formulary?
Not every hospital is legally required to have one, but most do - especially in states like Florida, where law 400.143 mandates formularies for nursing homes. Even in states without specific laws, most hospitals use formularies to control costs and reduce medication errors. Over 90% of long-term care facilities and nearly 80% of acute care hospitals use them.
Can a patient refuse a drug substitution?
Yes. Even if a drug is on the formulary and the substitution is legal, patients have the right to refuse. They can ask for the originally prescribed medication. The facility must document the refusal and notify the prescribing doctor. However, the doctor may need to justify why the non-formulary drug is medically necessary.
Why do formularies change so often?
Formularies are updated regularly because new evidence emerges - new studies, new side effects, new generic versions, or price changes. Florida law requires facilities to review their formularies quarterly. The American Society of Health-System Pharmacists now recommends bi-monthly reviews to keep up with fast-changing drug data.
How do formularies affect medication costs for patients?
Formularies don’t directly change what patients pay out of pocket - that’s handled by insurance. But they influence which drugs are available. If a cheaper generic is on the formulary, patients may get it instead of a brand-name drug, which could lower their co-pay. However, if a patient needs a non-formulary drug, they may face higher costs or delays getting approval.
Do formularies improve patient safety?
Studies show they can. In long-term care, evidence-based formularies reduce adverse drug events by 15-30% by eliminating high-risk combinations and promoting safer alternatives. However, poor communication around substitutions - especially during care transitions - can create new risks. Safety depends on how well the system is managed, not just whether it exists.


Comments
Priscilla Kraft
Just had my grandma switched from lisinopril to benazepril in her nursing home-no one told us. She got dizzy for 3 days. 😔 I asked why, and the nurse said, 'It's cheaper.' I get cost-saving, but not at the cost of her safety. 🤷♀️
January 11, 2026 at 15:15
Alex Smith
So let me get this straight-we’ve got a system designed to prevent errors, but it’s so opaque that patients are getting med changes without even knowing they happened? Classic. 🤦♂️
January 12, 2026 at 12:43
Madhav Malhotra
Interesting! In India, hospitals rarely have formal formularies-doctors just prescribe what they trust. But I’ve seen patients get confused when they come to the US and their meds 'disappear.' Maybe we need more transparency globally? 😊
January 13, 2026 at 15:02
Jason Shriner
So the hospital's 'pharma committee' is basically playing god with my meds... and I'm supposed to be grateful? 🙃
January 14, 2026 at 19:41
Alfred Schmidt
THIS IS WHY PEOPLE DIE IN HOSPITALS. NO ONE TELLS YOU. NO ONE DOCUMENTS IT. YOU’RE JUST A NUMBER ON A LIST. I’VE SEEN IT. MY MOM GOT SWITCHED TO A GENERIC THAT MADE HER SEIZURES WORSE. THEY DIDN’T EVEN NOTICE FOR TWO WEEKS. THIS IS A SCANDAL.
January 15, 2026 at 10:24
Sean Feng
Formularies are fine if you don’t care about patients
January 16, 2026 at 17:36
Vincent Clarizio
Look, I get the logic-reduce errors, cut costs, standardize care. But this system treats patients like variables in a spreadsheet. You can’t just swap out a drug like you’re swapping out a lightbulb. People aren’t widgets. Their bodies react differently. Their fears, their histories, their trust-all of it matters. And when you remove human judgment from the equation, you don’t get efficiency-you get a cold, bureaucratic machine that doesn’t know when to bend. The fact that nurses spend 30 hours a quarter just documenting substitutions instead of holding a patient’s hand? That’s not progress. That’s failure dressed up as policy. And don’t give me that ‘evidence-based’ crap. Evidence doesn’t care if your grandma’s terrified because she doesn’t know why her pills changed. The system needs empathy, not just algorithms.
January 17, 2026 at 05:45
Sam Davies
Oh, so now we’re outsourcing clinical decisions to a committee of pharmacists who’ve never met the patient? How quaint. I’m sure they’ve all read the 2024 Gartner whitepaper on AI-driven formularies. How terribly modern. 😌
January 17, 2026 at 14:59
Christian Basel
Therapeutic substitution is a formulary-driven, cost-optimized, evidence-based intervention aimed at reducing polypharmacy risk and enhancing pharmacoeconomic efficiency. The lack of interoperability between EHRs and formulary engines creates suboptimal clinical decision support, resulting in care fragmentation during transitions. We need dynamic, real-time formulary adaptation protocols.
January 19, 2026 at 08:14
Roshan Joy
My cousin’s in a rehab center and they changed her seizure meds without telling her family. She was fine until she started having episodes again. We found out by accident. I’m glad someone’s talking about this. Maybe we should all ask for the formulary list when we’re admitted? 🙏
January 20, 2026 at 11:17
Matthew Miller
Of course the system fails. It’s designed by bureaucrats who’ve never held a dying patient’s hand. They think ‘cost-efficiency’ is a virtue. It’s not. It’s negligence wrapped in a PowerPoint. This isn’t healthcare. It’s corporate insurance fraud with a lab coat.
January 20, 2026 at 17:26
Priya Patel
My aunt got switched from her heart med and didn’t say anything because she didn’t want to be ‘difficult.’ I’m so mad. We need to normalize asking ‘Why?’ and writing everything down. 💪❤️
January 21, 2026 at 10:38
Jennifer Littler
Formulary compliance metrics are being tied to CMS reimbursement? That’s the first step toward meaningful accountability. But until EHRs are interoperable and staff are trained to flag substitutions in real time, this is just performative compliance. We need clinical decision support embedded in the workflow-not bolted on as an afterthought.
January 21, 2026 at 18:06
Adewumi Gbotemi
Here in Nigeria, we don’t have these systems. Doctors just give what’s in stock. Sometimes it works. Sometimes it doesn’t. I think your system tries to be smart, but it forgets the person. Just talk to the patient. That’s all.
January 21, 2026 at 20:16