Why accurate cancer staging matters more than you think
Getting cancer staged right isn’t just a technical detail-it changes everything. A stage II tumor might be treated with surgery and chemo. A stage IV tumor? That’s when treatment shifts to managing the disease, not curing it. The difference between these stages often comes down to one thing: imaging. Three technologies-PET-CT, MRI, and PET-MRI-have become the backbone of modern cancer staging. But they’re not interchangeable. Each has strengths, weaknesses, and specific cancers where they shine. Choosing the wrong one can mean missed metastases, wrong treatment paths, or unnecessary radiation exposure.
PET-CT: The workhorse of oncology imaging
PET-CT became the standard in the early 2000s, and for good reason. It combines two scans into one: a PET scan that shows where cancer cells are metabolically active (using a sugar-based tracer called 18F-FDG), and a CT scan that maps out the body’s anatomy. Together, they tell doctors not just where a tumor is, but how aggressive it is.
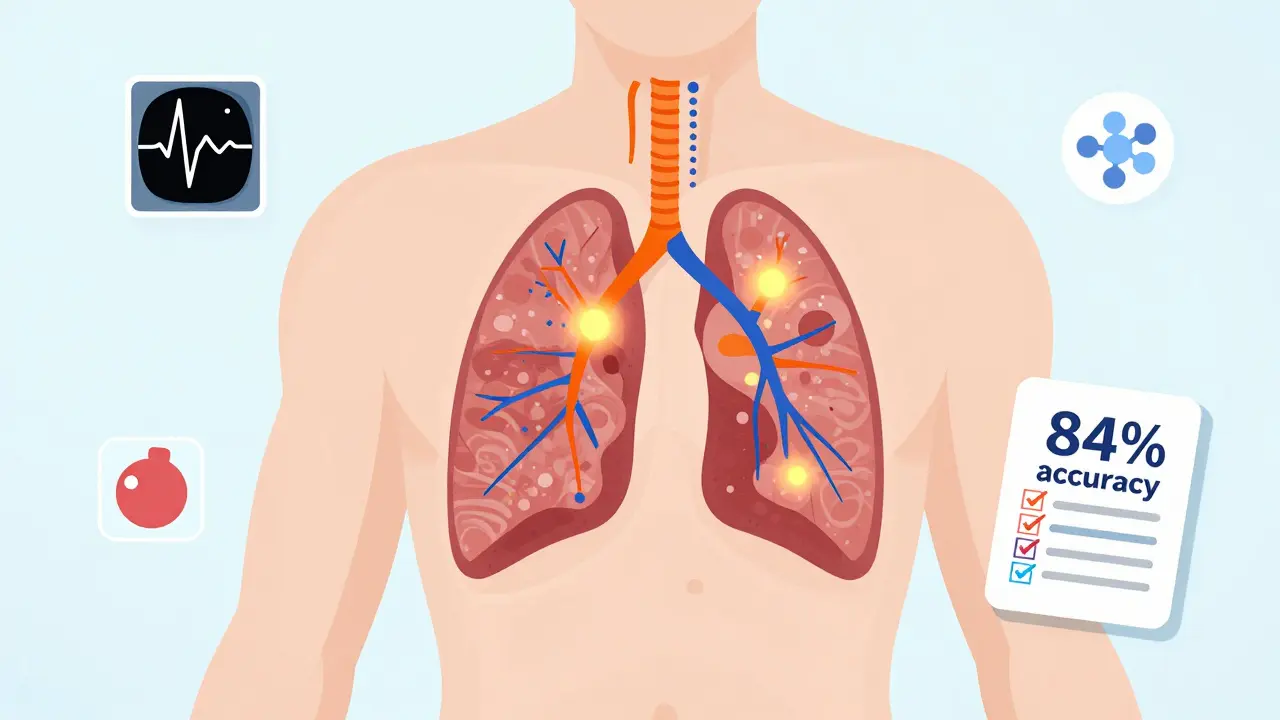
For lung cancer, lymphoma, and colorectal cancer, PET-CT is still the go-to. A 2023 meta-analysis found it correctly identified cancer spread in lymph nodes for non-small cell lung cancer with 84% accuracy. It’s fast-most scans take 15 to 20 minutes. Hospitals love it because it’s widely available and reimbursed by most insurance plans. A typical PET-CT system costs between $1.8 million and $2.5 million to install, and the radiation dose ranges from 10 to 25 mSv, which is higher than a standard CT but justified by the diagnostic payoff.
But it has limits. PET-CT struggles with cancers that don’t use a lot of sugar, like some prostate and liver tumors. It also can’t tell the difference between inflammation and cancer in some cases, leading to false positives. And while it’s great for finding tumors, it’s not as good at showing how they’re connected to nearby organs or nerves-something MRI does far better.
MRI: The detail master without radiation
MRI doesn’t use radiation. Instead, it uses powerful magnets and radio waves to create ultra-detailed images of soft tissues. For cancers in the brain, spine, liver, prostate, and pelvis, MRI is often the most accurate tool available. A 2022 study in Cancer showed that for prostate cancer, MRI detected tumors with 75% accuracy, compared to 62% for PSMA PET-CT. That’s because MRI can see the tiny changes in tissue structure that signal cancer, even when the tumor is too small to light up on a PET scan.
It’s also the best tool for checking if cancer has spread to the brain or spinal cord. In neuro-oncology, MRI alone can distinguish between tumor recurrence and radiation damage with 70-80% accuracy. That’s critical-mistaking scar tissue for a new tumor can lead to unnecessary surgery or radiation.
But MRI has downsides. It’s slow. A full-body or detailed pelvic MRI can take 30 to 60 minutes. Patients have to lie perfectly still. Movement ruins the images. It’s also not ideal for people with metal implants, pacemakers, or severe claustrophobia. And while MRI is great at showing anatomy, it doesn’t tell you how active the cancer is. That’s where PET comes in.
PET-MRI: The hybrid that’s changing the game
PET-MRI is the newest player, first approved in 2011 and still growing. It merges the metabolic power of PET with the soft-tissue clarity of MRI in a single scan. The result? A picture that shows both where the cancer is and how aggressively it’s behaving-all in one session.
It’s especially powerful for cancers where location and biology matter together. In liver cancer, a 2022 survey of radiologists found 68% felt PET-MRI gave them more confidence than PET-CT in telling benign lesions from metastases. For pediatric cancers, it’s a game-changer: less radiation over a lifetime means fewer long-term risks. In brain tumors, PET-MRI can differentiate recurrence from radiation necrosis with 85-90% accuracy, compared to 70-80% for MRI alone.
But it’s not perfect. The biggest problem? Time. A PET-MRI scan takes 45 to 60 minutes. That’s a challenge for frail patients or those in pain. Motion during the scan can blur the images. Also, PET-MRI requires special software to correct for how the magnetic field affects the PET signal-a technical hurdle that still causes artifacts in 63% of centers, according to a 2022 study.
Cost is another barrier. A PET-MRI machine runs $3 million to $4.2 million-nearly double the price of a PET-CT. And because it’s newer, insurance reimbursement isn’t always guaranteed. Still, adoption is rising. Academic hospitals in the U.S. and Europe are leading the way, with 78% of PET-MRI installations in teaching centers. The technology is expected to grow at 18.7% per year through 2030, according to Signify Research.
Which scan for which cancer?
There’s no one-size-fits-all. The best imaging choice depends on the cancer type, location, and what question the doctor needs answered.
- Breast cancer: For checking response to chemo before surgery, PET-CT has higher specificity than MRI, meaning fewer false alarms. But MRI is better at spotting small tumors in dense breast tissue.
- Prostate cancer: PSMA PET-CT is great for finding distant spread. But for local staging-whether the cancer is still inside the prostate or has broken through its capsule-MRI is the gold standard.
- Pancreatic cancer: A 2023 study showed PET-MRI changed treatment plans for nearly half of patients because it found hidden tumors that PET-CT missed.
- Lymphoma: PET-CT remains the standard for staging and checking if treatment worked. PET-MRI is being studied but hasn’t replaced it yet.
- Brain tumors: PET-MRI is becoming the preferred tool because it can tell if a new lesion is cancer returning or just scar tissue from past radiation.
- Pediatric cancers: PET-MRI is preferred when possible to avoid radiation exposure over a child’s lifetime.

What doctors really think
Experts don’t see these tools as rivals-they see them as partners. Dr. Richard L. Wahl from Johns Hopkins says PET-MRI is “particularly valuable for pelvic malignancies and CNS tumors,” but adds that PET-CT remains the workhorse for most cases because it’s faster and more available.
A 2019 consensus from European nuclear medicine and MRI societies concluded PET-MRI offers “moderate advantages” in specific cases but isn’t a universal replacement. Dr. Hedvig Hricak from Memorial Sloan Kettering puts it bluntly: “The choice must be personalized.”
Cost is a real concern. PET-MRI can cost $2,500 to $3,500 per scan in the U.S., compared to $1,600-$2,300 for PET-CT. That’s why many centers use PET-MRI selectively-for complex cases where the extra detail will change treatment.
What’s next for oncologic imaging?
The future isn’t just about better machines-it’s about smarter interpretation. In January 2024, Siemens cleared a new PET-MRI system that cuts scan time to just 6 minutes for a full-body scan. That’s a huge leap forward.
Artificial intelligence is also stepping in. At the 2023 RSNA meeting, researchers showed AI models that could predict how a tumor would respond to treatment just by analyzing PET-MRI images. The NCI’s PREDICT trial is now testing whether AI can personalize imaging choices based on a tumor’s genetic profile.
Novel tracers are expanding what PET can see. PSMA for prostate cancer, DOTATATE for neuroendocrine tumors, and others are making PET scans more specific. When paired with MRI’s detail, these tracers are creating a new level of precision.
One thing is clear: the future of cancer care is multimodal. Doctors won’t choose one scan over another-they’ll use them together, in sequence, to build a complete picture. The goal isn’t just to find cancer. It’s to understand it deeply enough to beat it.
What patients should know
If you’re facing cancer staging, ask your oncologist: “Which imaging test are you recommending, and why?” Don’t assume PET-CT is always the best. Ask if MRI or PET-MRI might give a clearer answer for your specific cancer. If you’re a child, young adult, or need multiple scans over time, radiation exposure matters. Ask if a non-radiation option like MRI is feasible.
Don’t be afraid to ask about wait times, costs, and whether the facility has experience with the specific scan you need. Not all centers are equally skilled with PET-MRI. Experience matters.

Comments
Gaurav Meena
This is such a game-changer for patients like my cousin who just got diagnosed with prostate cancer. MRI saved her from unnecessary biopsies. Seriously, if you're in a situation like this, ask for the right scan - it matters more than you think. 🙌
February 1, 2026 at 04:11
Natasha Plebani
The epistemological rupture between metabolic activity and structural morphology in oncologic imaging represents a paradigmatic shift in diagnostic ontology. PET-MRI’s multimodal convergence transcends reductionist biomarker logic, enabling a phenomenological mapping of tumor ecology that reconfigures therapeutic intentionality. The spatial-temporal resolution differential between FDG-PET and PSMA-targeted tracers demands a hermeneutic framework beyond conventional radiological semiotics.
February 1, 2026 at 21:17
Rob Webber
Stop pretending PET-MRI is some miracle machine. It’s overpriced, slow as molasses, and half the hospitals can’t even calibrate it right. PET-CT does 90% of the job for a third of the cost. If your oncologist is pushing PET-MRI without a clear reason, they’re either trying to pad their budget or they don’t know what they’re doing. Wake up people.
February 1, 2026 at 22:59
calanha nevin
The data clearly supports selective use of PET-MRI in complex cases where anatomical detail and metabolic activity must be correlated to avoid misclassification. For pediatric patients and recurrent CNS tumors, the reduction in cumulative radiation exposure justifies the cost and time investment. Clinical judgment must guide imaging selection not protocol inertia
February 2, 2026 at 21:53
Lisa McCluskey
I’ve seen too many patients get stuck in imaging limbo because no one explained why one test was chosen over another. It’s not about which tech is better it’s about which one answers the right question for that person. Ask why. Know your options. You deserve that clarity
February 3, 2026 at 00:45
owori patrick
In Nigeria we barely have access to CT scans let alone PET-MRI. But reading this makes me hopeful. Maybe one day our hospitals can afford these tools. Until then, we rely on what we have and pray it’s enough. Thank you for writing this with such honesty
February 4, 2026 at 02:13
Claire Wiltshire
The integration of novel tracers such as DOTATATE and PSMA with high-resolution MRI represents a significant advancement in precision oncology. It is imperative that clinicians remain informed about these developments to ensure optimal patient outcomes. Access and equity must remain central to the conversation surrounding adoption
February 6, 2026 at 00:11
Darren Gormley
LMAO this article is just a Siemens ad. PET-MRI is 63% artifact-ridden and only used in fancy academic hospitals because they have the money to waste. Meanwhile real hospitals are using PET-CT to save lives. Also why is everyone acting like MRI doesn’t have contraindications? Pacemakers? Metal implants? Yeah good luck with that. 😂
February 7, 2026 at 16:28
Mike Rose
I dont even know what half these words mean but i know pet ct is what they use and its fine. why do they need to spend so much on fancy machines when the old one works? also why is everyone so into mri like its magic? its just a loud tube
February 8, 2026 at 17:29
Russ Kelemen
This is the kind of post that reminds me why I got into medicine. It’s not about the tech - it’s about the person behind the scan. A kid in India, a veteran with a pacemaker, a woman with dense breast tissue - they all need different answers. The real innovation isn’t the machine. It’s the doctor who takes the time to ask, 'What’s your story?'
February 8, 2026 at 17:58
Diksha Srivastava
I’m so glad someone finally wrote this in plain language. My sister’s oncologist skipped MRI and went straight to PET-CT - turned out the tumor was hidden in dense tissue. She’s doing great now. Always ask. Always push. You’ve got this 💪
February 10, 2026 at 14:27