Starting a new medication can feel overwhelming. You’ve been told it will help, but you’ve also heard about the side effects-nausea, dizziness, fatigue, or worse. What if you could avoid those rough first weeks? The answer isn’t to skip the medicine. It’s to start slow.
Why Slow Up-Titration Works
Slow up-titration means starting with a tiny dose of a medication and slowly increasing it over weeks or months. It’s not about being cautious-it’s about biology. Your body doesn’t react well to sudden changes. When you jump straight to a full dose of a GLP-1 agonist like semaglutide, your gut goes into shock. Up to 65% of people get nauseous, vomit, or lose their appetite. But if you start at 0.25mg once a week and wait four weeks before increasing, that number drops to under 20%. That’s not luck. That’s your receptors adapting. This isn’t just for weight-loss drugs. It’s standard for heart failure medications like beta-blockers and ACE inhibitors. In the 1980s, doctors noticed patients were quitting their meds because they felt awful. One study found only 12% could handle full-dose metoprolol right away. When they started at 6.25mg and crept up over six weeks, 83% stayed on it. That’s the difference between treatment failure and life-changing results.How Slow Titration Schedules Vary by Drug
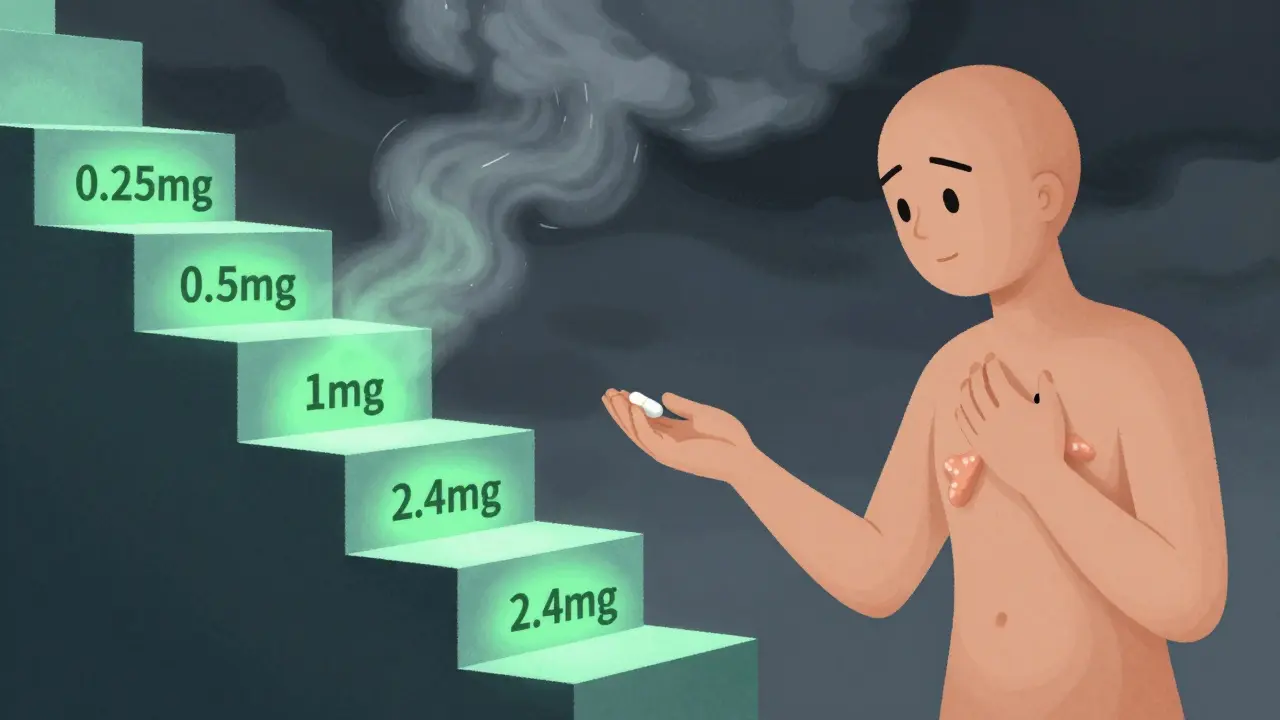
Not all medications need the same pace. The schedule depends on how the drug works and how harsh its side effects are.- GLP-1 agonists (semaglutide, liraglutide): These take the longest. For injectable semaglutide, you start at 0.25mg weekly for four weeks, then move to 0.5mg for four more weeks, then 1mg, and finally up to 2.4mg. The whole process takes 16 to 20 weeks. The oral version follows a 60-day ramp-up: 3mg for 30 days, then 7mg, then 14mg.
- Beta-blockers (metoprolol, carvedilol): Used for heart failure and high blood pressure. Doses are usually doubled every two to four weeks. You might start at 3.125mg twice daily and work up to 25mg or more over 8 to 12 weeks.
- ACE inhibitors (lisinopril, enalapril): Often started at 2.5-5mg daily, then increased every 1-2 weeks. The goal is to reach 10-40mg without dropping blood pressure too low.
- Antidepressants (SSRIs like sertraline): Even here, slow titration helps. Starting at 25mg instead of 50mg reduces early anxiety and insomnia, making it easier to stick with the treatment.
Some drugs, like SGLT2 inhibitors (empagliflozin, dapagliflozin), don’t need titration at all. They’re safe to start at full dose. That’s why patients often ask: “Why can’t all diabetes meds be like this?” The answer? Not all drugs are built the same. GLP-1s hit your gut hard. Beta-blockers slow your heart too fast if you start high. Titration isn’t arbitrary-it’s science.
The Real Benefits: Adherence and Survival
The goal isn’t just to feel better. It’s to stay alive. A 2021 meta-analysis in JAMA Internal Medicine showed that slow titration increased medication adherence by 37% compared to starting at full dose. That’s huge. If you quit your heart failure meds because you felt sick, your risk of hospitalization or death goes up. Slow titration cuts that risk. The PARADIGM-HF trial showed a 52% drop in severe side effects when patients followed structured titration. The SUSTAIN FORTE trial found GI side effects fell from 45% to 18% when semaglutide was titrated properly. And in heart failure, following titration protocols reduced all-cause mortality by 35%, according to Dr. John McMurray’s work in the European Heart Journal. It’s not just numbers. Real people say it’s life-changing. On Reddit, one user wrote: “Starting semaglutide at 0.25mg saved me. I tried skipping the titration once-I threw up for three days and quit. This time, I stuck with it. I’ve lost 40 pounds and feel like myself again.”
The Downsides: Time, Complexity, and Burnout
There’s no free lunch. Slow titration has real costs. First, it takes time. You might be on a low dose for months before you feel the full benefit. For someone with an HbA1c of 9.5%, waiting six months to reach full glucose control can feel unbearable. Dr. Robert Lash warns that for drugs like metformin-which are very safe-delaying the full dose can do more harm than good. Second, it’s complicated. Patients have to remember when to increase their dose, track symptoms, and schedule frequent check-ins. A 2021 study found that 22% of patients over 65 struggled with the multiple dose changes. That’s why tools like Medisafe, a pill reminder app, help. Users who used it had 18% higher adherence. And it’s not just patients. Doctors are stretched thin. A 2022 Mayo Clinic study found providers spend nearly 13 minutes per visit explaining titration. With 2.3 extra visits per patient during the process, the system is under pressure. The American Medical Association estimates that managing multiple titration schedules could add 4.7 hours of work per week per complex patient.What You Should Do: A Practical Guide
If you’re starting a medication that requires slow titration, here’s how to make it work:- Know your schedule. Don’t guess. Ask your doctor for a written plan: what dose, when to increase, what symptoms to watch for.
- Use a tracker. Write down your dose each week. Note side effects. Did you feel dizzy? Nauseous? Sleep better? This helps your doctor adjust faster.
- Follow the 2-week rule. If a side effect lasts more than two weeks at your current dose, don’t push through. Call your provider. It might mean you need to stay at that dose longer-or switch.
- Don’t skip doses. Missing a dose during titration can mess up your rhythm. If you forget, don’t double up. Call your pharmacy or doctor for advice.
- Ask about support tools. Are there apps? Telehealth check-ins? Nurse hotlines? Many clinics now offer digital titration programs. Omada Health’s GLP-1 program reduced dropouts by 41% in a pilot study.
And if you’re on multiple medications that require titration? Talk to your doctor about sequencing. Don’t start three new drugs at once. Tackle one at a time.

What’s Next: AI and Personalized Titration
The future of titration isn’t one-size-fits-all. Companies like Verily and Novo Nordisk are building AI models that predict how you’ll react to a drug based on your genetics, weight, and even gut microbiome. Early results show they can predict side effect risk 28% better than current methods. In 2023, the American College of Cardiology launched TARGET-HF, a standardized heart failure titration protocol requiring biweekly telehealth visits. More clinics are adopting these models because they work. But here’s the big question: will healthcare systems be able to keep up? If every patient on a GLP-1, beta-blocker, and ACE inhibitor needs weekly check-ins, we’re looking at a massive strain on resources. Some experts are already asking: which drugs truly need slow titration? Maybe SGLT2 inhibitors don’t. Maybe metformin doesn’t. The goal isn’t to slow everything down-it’s to slow the right things down, just enough.Final Thought: It’s Not About Patience. It’s About Power.
Slow titration isn’t about waiting. It’s about taking control. You’re not just taking a pill. You’re teaching your body to accept it. You’re reducing the chance of quitting. You’re increasing your odds of living longer, feeling better, and staying on track. It’s not easy. But it’s worth it. The science is clear. The stories are real. And for many, it’s the difference between giving up-and turning things around.Why can’t I just start at the full dose of my new medication?
Starting at full dose can overwhelm your body’s systems, especially with drugs that affect your gut, heart, or nervous system. For example, GLP-1 agonists cause nausea in up to 65% of people at full dose-but only 18% when titrated slowly. Rapid dosing leads to higher dropout rates, not faster results. Your body needs time to adapt.
How long does slow titration usually take?
It depends on the drug. GLP-1 agonists like semaglutide can take 16-20 weeks to reach the highest dose. Beta-blockers for heart failure often take 8-12 weeks. Some medications, like SGLT2 inhibitors, don’t require titration at all. Always follow your provider’s schedule-don’t assume all drugs work the same way.
What should I do if side effects don’t go away after two weeks?
Don’t push through. Contact your doctor. Side effects that last beyond two weeks may mean you need to stay at your current dose longer, reduce the dose temporarily, or switch medications. The goal isn’t to suffer through it-it’s to find the dose that works for you without unnecessary discomfort.
Is slow titration only for chronic conditions?
Mostly, yes. Slow titration is used for long-term treatments like heart failure, diabetes, depression, and weight management. It’s not used in emergencies-like high blood pressure spikes-where fast-acting drugs are needed immediately. Titration is about sustainable, safe long-term use.
Can I speed up my titration schedule if I feel fine?
No. Feeling fine doesn’t mean your body has adapted. Side effects can appear later, or you might be at risk for low blood pressure, kidney stress, or heart rhythm issues. Always follow your provider’s schedule. Even if you feel great, skipping steps can lead to serious complications down the road.
Are there apps or tools to help me keep track of my titration?
Yes. Apps like Medisafe, MyTherapy, and Dosecast send reminders for dose changes and let you log side effects. Some clinics offer digital titration programs linked to your electronic record. These tools improve adherence by up to 18% and help your doctor spot issues before they become problems.
Why do some medications not need titration at all?
Some drugs, like SGLT2 inhibitors (e.g., Jardiance) or metformin, have wide safety margins and mild side effects that don’t worsen with higher doses. Clinical trials show they’re safe to start at full dose. Titration is only needed when the risk of side effects is high at the start-like with drugs that affect your gut, heart rate, or blood pressure.
Will my insurance cover the extra doctor visits needed for titration?
Many do, especially under value-based care models. Accountable care organizations and Medicare Advantage plans often cover telehealth check-ins during titration because they reduce hospitalizations. Check with your provider or insurer. If you’re in a program like TARGET-HF, visits are typically included as part of your care plan.
Next steps: If you’re starting a new medication, ask your doctor for a written titration plan. Write down your doses and symptoms. Use a reminder app. And if you’re unsure about anything-call. You’re not just taking a pill. You’re managing your health, one small step at a time.

Comments
Ajay Brahmandam
I've been on metoprolol for heart failure for 3 years now. Started at 3.125mg, took 10 weeks to get to 25mg. Felt like a snail but I'm still here. No hospital visits since. Slow wins the race. 🙌
December 22, 2025 at 04:06
Gabriella da Silva Mendes
Why do we even need this? 🤔 Big Pharma just wants you to see the doctor more. I started semaglutide at 1mg. Threw up once. Didn't care. Lost 50lbs in 4 months. Who needs science when you got grit?
December 23, 2025 at 04:45
Jeremy Hendriks
Titration isn't science. It's control. They want you dependent. They want you checking in. They want you afraid to go off-script. What if the real side effect is the system itself?
December 23, 2025 at 13:15
Sam Black
I work with diabetics in rural Australia. Most don't even know what 'titration' means. We hand-write schedules on napkins. Some use WhatsApp reminders. It’s messy. But it works. Don't underestimate low-tech solutions.
December 25, 2025 at 07:52
Aliyu Sani
The gut-brain axis is the real MVP here. When you hit GLP-1s hard, you're not just nauseous-you're signaling existential distress to your vagus nerve. Slow titration? It's neurobiological diplomacy. Let the body negotiate.
December 26, 2025 at 19:38
Kathryn Weymouth
I'm a nurse. I've seen people quit meds because they thought 'feeling awful' meant it was working. It doesn't. Side effects are warnings, not milestones. This post saved three patients this month alone.
December 28, 2025 at 00:12
Julie Chavassieux
I tried to speed up my semaglutide... and I ended up in the ER... with dehydration... and a panic attack... and my cat staring at me like I betrayed her... I'm never doing that again...
December 28, 2025 at 07:56
Kiranjit Kaur
My cousin in Delhi started metformin at 1000mg. Got dizzy. Quit. Then came back 6 months later with HbA1c at 11.5. Started slow this time. Now she hikes every weekend. Patience isn't passive-it's power.
December 28, 2025 at 20:00
Sai Keerthan Reddy Proddatoori
This is just the government letting big pharma control us. Why not just give us the real dose? Why make us wait? They want us weak. They want us docile. Wake up people.
December 30, 2025 at 07:02
jenny guachamboza
I think the FDA is hiding something... why do only SOME drugs need titration? Why not all? Maybe they're testing something on us... remember when they said vaccines were safe? 🤫👁️
December 31, 2025 at 12:21
Nader Bsyouni
The real question isn't how to titrate it's whether we should be taking these drugs at all. We've turned biology into a spreadsheet. We've outsourced healing to algorithms. What happened to listening to our bodies?
December 31, 2025 at 23:51
Tony Du bled
My dad’s from Nigeria. He didn’t believe in pills. Started him on lisinopril at 2.5mg. Told him to write down how he felt every day. He did. For 6 months. Now he’s hiking in Abuja. No meds needed anymore. Sometimes the body just needs time.
January 1, 2026 at 00:43
Tarun Sharma
Adherence improves with structured titration. Evidence-based. No speculation required.
January 2, 2026 at 10:13
Jim Brown
To titrate is to honor the architecture of the human organism. We are not machines to be calibrated with brute force. We are symphonies of adaptation-each note, each dose, a whisper to the cellular self. To rush is to deafen the soul.
January 3, 2026 at 02:09
Candy Cotton
I read this entire article. Took me three days. I printed it. Highlighted it. Made a flowchart. I’m not taking any chances. If you’re not tracking your side effects in a color-coded Excel sheet, you’re not serious about your health.
January 3, 2026 at 18:51