When it comes to HPV prevention, the practice of reducing the risk of infection by the human papillomavirus through vaccination, screening, and safe behaviors. Also known as human papillomavirus protection, it’s one of the most effective ways to stop cervical cancer before it starts. HPV isn’t just a women’s health issue—it affects everyone. About 80% of sexually active people will get at least one type of HPV in their lifetime. Most infections clear on their own, but some stick around and can lead to cancer. That’s why prevention isn’t optional—it’s essential.
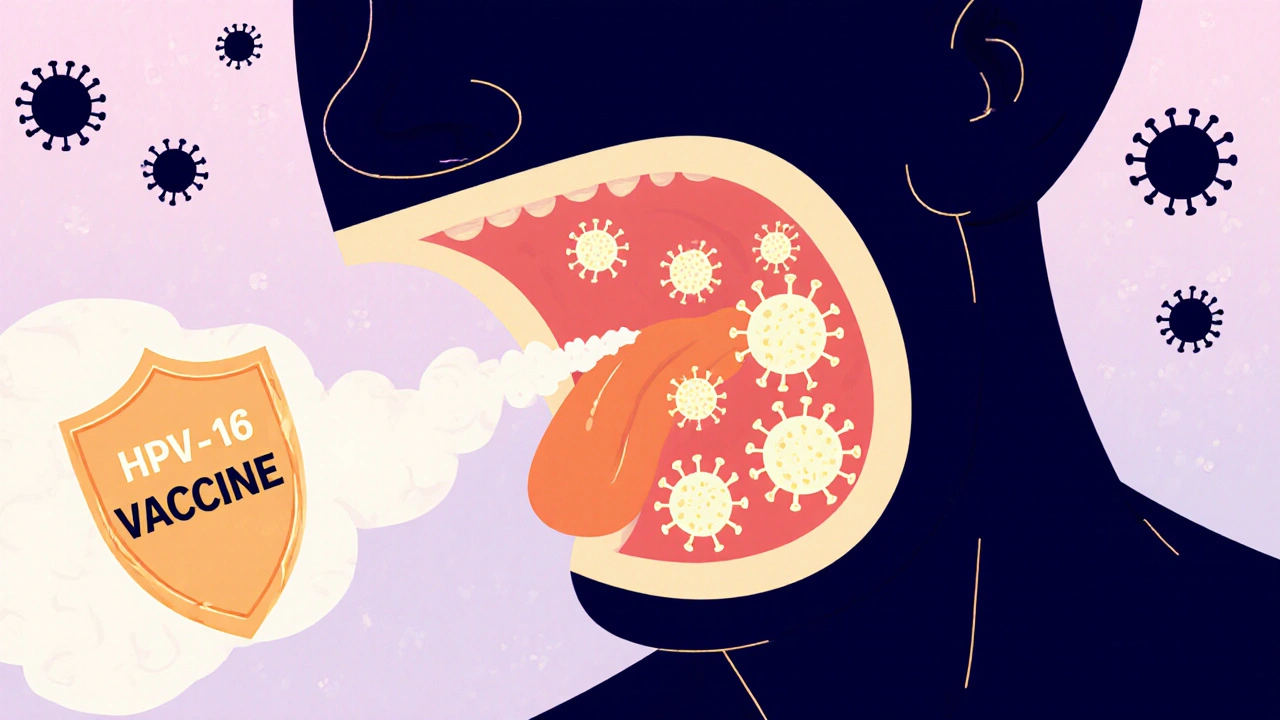
The cornerstone of HPV prevention, the practice of reducing the risk of infection by the human papillomavirus through vaccination, screening, and safe behaviors. Also known as human papillomavirus protection, it’s one of the most effective ways to stop cervical cancer before it starts. is the HPV vaccine, a safe and highly effective immunization that protects against the strains of HPV most likely to cause cancer and genital warts. Also known as Gardasil, it works best when given before exposure, ideally between ages 9 and 12. But it’s not just for kids. Adults up to age 45 can still benefit, especially if they haven’t been fully vaccinated. The vaccine doesn’t treat existing infections, but it stops new ones. That means even if you’ve had HPV before, getting vaccinated can protect you from other dangerous types.
Cervical cancer, a preventable disease caused by persistent infection with high-risk HPV strains, primarily types 16 and 18. Also known as HPV-related cancer, it develops slowly, often over years, and is almost always detectable through routine screening. Regular Pap smears and HPV tests catch abnormal cells before they turn cancerous. Many people skip these tests because they feel fine—but HPV doesn’t always cause symptoms. That’s why prevention isn’t just about shots. It’s about showing up for checkups, even when nothing feels wrong.
Condoms help reduce transmission, but they don’t block all HPV because the virus lives on skin not covered by a condom. That’s why vaccination plus screening is the real double shield. And while HPV is common, it’s not inevitable. You can lower your risk by limiting partners, staying up to date on vaccines, and getting tested. There’s no magic pill, but there are proven steps—and they work.
What you’ll find below are real, practical guides on how HPV prevention plays out in daily life—from understanding vaccine schedules to spotting warning signs that don’t get talked about enough. These aren’t theory pieces. They’re based on what people actually experience when they navigate testing, treatment, and long-term protection. Whether you’re wondering why your doctor pushed the vaccine, how to talk to a partner about HPV, or what happens if you miss a dose, the answers are here—no jargon, no fearmongering, just what you need to know.
Posted by
Jenny Garner
13 Comments
HPV causes throat, anal, and other cancers - but they’re preventable. Learn how the HPV vaccine works, who needs it, and why screening still matters for women. Most cases are avoidable with simple steps.
read more