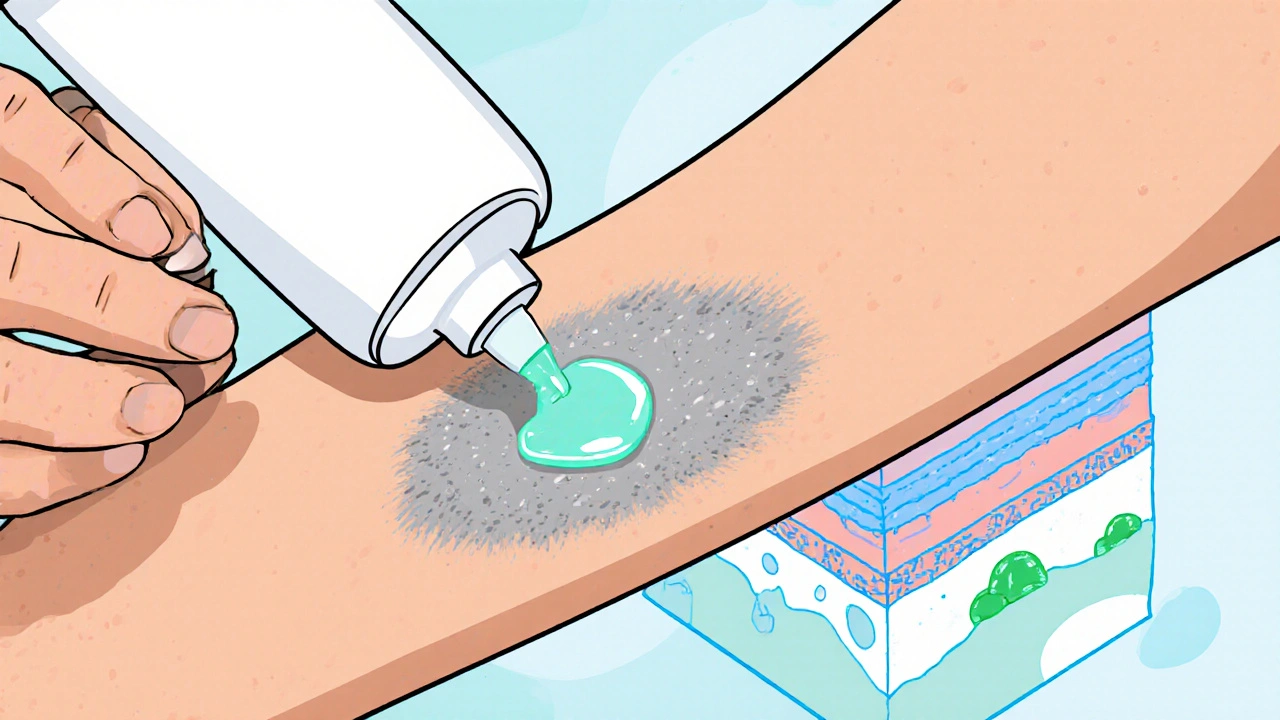
When managing psoriasis treatment, the range of medical approaches used to control the chronic, immune‑driven skin disorder psoriasis. Also called psoriasis therapy, it relies on several key strategies. Topical corticosteroids, first‑line creams that calm inflammation and reduce scaling form the backbone for mild to moderate flare‑ups; they act quickly, are cheap, and can be applied at home, but long‑term use may thin skin. Biologic drugs, injectable agents that target specific immune pathways like TNF‑α or IL‑17 are reserved for moderate‑to‑severe cases and have reshaped long‑term management; they offer high clearance rates yet require lab monitoring and can be pricey. Phototherapy, controlled exposure to UVB or PUVA light that slows skin cell growth offers a non‑systemic alternative when creams alone fall short; regular clinic visits are needed, and over‑exposure can raise skin‑cancer risk. Finally, Systemic oral medications, such as methotrexate or cyclosporine, suppress the overactive immune response from within provide another route for extensive disease; they are effective but can affect liver, kidneys, or blood counts, so routine tests are mandatory. Together these options illustrate that psoriasis treatment requires a tailored mix of skin‑direct and immune‑focused tactics, and the choice often hinges on disease severity, patient lifestyle, and safety profile.
Choosing the right approach starts with a clear picture of how the skin looks, how often flare‑ups happen, and what everyday activities matter most to you. A dermatologist’s assessment influences treatment success, because the specialist can match the severity score to the most appropriate option. For many, starting with topical steroids and adding lifestyle tweaks—like stress reduction, moisturizing, and a balanced diet—keeps lesions in check without moving to aggressive therapy. If those steps fail, stepping up to phototherapy or a biologic often yields faster clearance, but patients need to weigh insurance coverage, injection comfort, and long‑term monitoring. Some people find that systemic oral meds work best for joint involvement (psoriatic arthritis), while others avoid them due to liver concerns and prefer biologics instead. Across all choices, patient education is a key driver: knowing potential side‑effects, how often to apply or take medication, and when to call the doctor creates a partnership that makes treatment more sustainable.
Below you’ll find detailed articles that dive deeper into each option, side‑effects, and practical tips to help you take control of your skin and feel confident about the path you choose.
Posted by
Jenny Garner
10 Comments
Discover the top 10 benefits of calcipotriol for psoriasis, from fast plaque clearance to long‑term safety, plus usage tips and FAQs.
read more