Understanding Idiopathic Orthostatic Hypotension and Chronic Fatigue Syndrome
Before diving into the relationship between Idiopathic Orthostatic Hypotension (IOH) and Chronic Fatigue Syndrome (CFS), it is essential to understand these two conditions individually. IOH is a form of low blood pressure that occurs when standing up from a sitting or lying position, leading to symptoms such as dizziness, lightheadedness, and fainting. Chronic Fatigue Syndrome, on the other hand, is a complex disorder characterized by extreme fatigue that doesn't improve with rest and may worsen with physical or mental activity.
Both conditions have a significant impact on an individual's quality of life, making it crucial to explore the potential connection between them. In this article, I will discuss the relationship between Idiopathic Orthostatic Hypotension and Chronic Fatigue Syndrome, shedding light on their commonalities, differences, and potential treatment options.
Common Symptoms of IOH and CFS
Although IOH and CFS are distinct medical conditions, they share several symptoms that can make it difficult to differentiate between the two. Some common symptoms include fatigue, dizziness, lightheadedness, and difficulty concentrating. These overlapping symptoms may lead to misdiagnosis or delay in receiving the appropriate treatment.
However, it is essential to note that while some symptoms may overlap, IOH and CFS have distinct diagnostic criteria. For example, IOH is primarily characterized by a drop in blood pressure upon standing, while CFS involves persistent fatigue that is not relieved by rest.
Orthostatic Intolerance in Chronic Fatigue Syndrome
One possible link between IOH and CFS is the presence of orthostatic intolerance (OI) in many individuals with CFS. Orthostatic intolerance is an inability to tolerate the upright posture without developing symptoms such as dizziness, lightheadedness, and fainting. Many CFS patients report worsening of their fatigue and other symptoms upon standing, which may be due to OI.
IOH is one of the most common forms of OI, which could explain the connection between these two conditions. Some researchers suggest that IOH may be a contributing factor to CFS or may even be a subtype of the disorder. However, more research is needed to establish this connection definitively.
Autonomic Nervous System Dysfunction
Another potential link between IOH and CFS is dysfunction of the autonomic nervous system (ANS), which regulates essential body functions such as heart rate, blood pressure, digestion, and body temperature. Both IOH and CFS have been associated with ANS dysfunction, although the exact nature of this dysfunction may differ between the two conditions.
For example, IOH is often linked to impaired functioning of the ANS in regulating blood pressure upon standing, while CFS patients may experience a more generalized dysfunction of the ANS, leading to a wide range of symptoms. Understanding the role of the ANS in both conditions could lead to better diagnostic tools and treatment options.
Comorbidity of IOH and CFS
Comorbidity, or the presence of multiple medical conditions in a single individual, may also play a role in the relationship between IOH and CFS. Some studies have found a higher prevalence of IOH in individuals with CFS compared to the general population, suggesting a possible connection between the two conditions.
However, it is important to note that comorbidity does not necessarily imply causation. In other words, just because IOH and CFS may frequently occur together does not mean that one condition causes the other. Further research is needed to determine the nature of this relationship and whether treating one condition may improve the symptoms of the other.
Diagnosing IOH and CFS
Given the overlapping symptoms and potential comorbidity of IOH and CFS, accurate diagnosis is crucial for effective treatment. To diagnose IOH, doctors will typically measure blood pressure while the patient is lying down and then again after standing for a few minutes. A significant drop in blood pressure upon standing may indicate IOH.
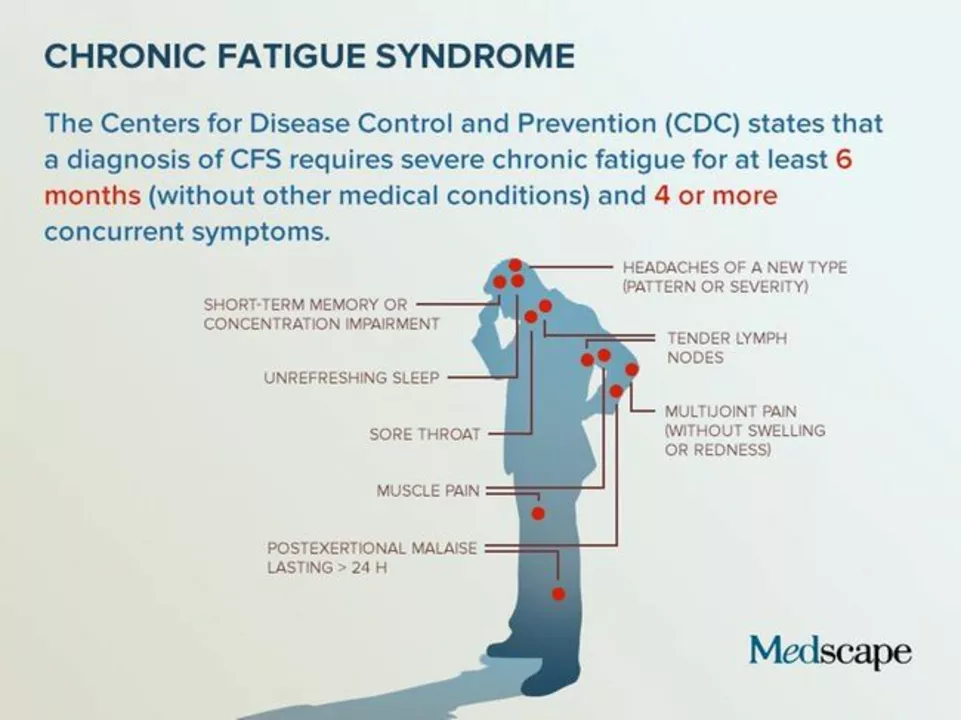
Diagnosing CFS can be more challenging, as there is currently no specific diagnostic test for the condition. Instead, doctors rely on a thorough evaluation of the patient's medical history, symptoms, and the exclusion of other potential causes of fatigue to make a diagnosis.
Treatment Options for IOH and CFS
Although there is no cure for either IOH or CFS, various treatment options can help manage symptoms and improve the quality of life. For IOH, treatments may include increasing fluid and salt intake, wearing compression stockings, and taking medications to raise blood pressure. Lifestyle changes, such as avoiding long periods of standing and elevating the head of the bed, may also be beneficial.
For CFS, treatment typically focuses on managing symptoms and may include sleep management, activity pacing, pain relief, and counseling to help cope with the emotional impact of living with a chronic condition. Some CFS patients may also benefit from medications to alleviate specific symptoms, such as antidepressants or anti-anxiety medications.
Future Research and the Importance of Awareness
Although the exact relationship between IOH and CFS remains unclear, research in this area is essential for improving our understanding of these complex conditions and developing more effective treatment options. By raising awareness of the potential link between IOH and CFS, we can encourage more research in this area and ensure that individuals affected by these conditions receive the appropriate care and support they need.

Comments
Meredith Blazevich
Feeling the overlap between idiopathic orthostatic hypotension and chronic fatigue syndrome really brings home how interconnected our bodies are. When you stand up and your blood pressure drops, the resulting dizziness can mimic the brain fog many CFS patients describe. That shared sensation often leaves clinicians wondering which condition is the primary driver. The autonomic nervous system, which orchestrates blood pressure regulation, also influences sleep cycles and energy metabolism, linking the two disorders in a subtle dance. Many patients report that a simple posture change can trigger a cascade of fatigue, hinting at a common physiological thread. Research suggests that orthostatic intolerance may amplify the already depleted energy reserves seen in CFS, creating a feedback loop of worsening symptoms. Moreover, the stress of living with unpredictable fainting episodes can exacerbate the emotional toll of chronic fatigue. Studies have found a higher prevalence of IOH among CFS cohorts, though causality remains elusive. Some clinicians advocate for a combined treatment approach, targeting both blood pressure stabilization and pacing strategies to break the cycle. Increasing fluid and salt intake, as well as compression garments, can mitigate the drop in pressure, potentially easing the fatigue burden. Meanwhile, cognitive-behavioral techniques and graded exercise therapy aim to improve autonomic resilience. It’s crucial for patients to receive a thorough evaluation that considers both diagnoses, rather than attributing all symptoms to one condition. Education about the link empowers individuals to advocate for comprehensive care. Ultimately, unraveling this relationship could open doors to novel therapeutic pathways that address the root of autonomic dysfunction. The journey to clarity is ongoing, but each shared insight brings us closer to meaningful relief.
May 27, 2023 at 20:30
Nicola Gilmour
Seeing how fluid intake can make a difference really motivates me to keep tweaking daily habits. Small steps like sipping electrolyte drinks before getting up can smooth out those dizzy spells, and that consistency builds confidence over time.
June 4, 2023 at 03:30
Darci Gonzalez
Focusing on posture adjustments can be a game changer for those with orthostatic issues. Try elevating the head of the bed a few inches and avoid standing still for too long. These simple moves often reduce the blood pressure dip and help sustain energy throughout the day
June 11, 2023 at 10:30
Marcus Edström
Building on that, incorporating low‑impact activities like gentle yoga can support autonomic balance without overtaxing the system. Consistency is key, and hearing success stories from the community reinforces the approach.
June 18, 2023 at 17:30
kevin muhekyi
Great tips, thanks!
June 26, 2023 at 00:30
Teknolgy .com
Isn't it amusing how we chase obscure physiological links while the market sells miracle supplements? 🤔 The allure of a one‑size‑fits‑all cure is a seductive illusion. Perhaps the real answer lies in accepting the complexity rather than simplifying it into a headline.
July 3, 2023 at 07:30
Caroline Johnson
Wow!!! This is exactly what the medical community needs-more clarity!!! The over‑reliance on vague explanations only fuels patient frustration!!! We must demand rigorous, data‑driven studies!!!
July 10, 2023 at 14:30
Megan Lallier-Barron
Honestly, I think the whole focus on autonomic dysfunction is overstated. If you look at the broader psychosocial factors, they often dominate the symptom picture. It's a classic case of moving the goalposts.
July 17, 2023 at 21:30
Kelly Larivee
True, stress does matter a lot. Simple breathing exercises can help calm the nervous system.
July 25, 2023 at 04:30
Emma Rauschkolb
From a neuroimmunological perspective, the interplay of cytokine signaling and baroreflex sensitivity is crucial. Dysregulation in these pathways manifests as both orthostatic intolerance and chronic fatigue phenotypes. Targeted modulation could yield therapeutic dividends. 😉
August 1, 2023 at 11:30
Kaushik Kumar
Absolutely! Coordinated care-combining lifestyle adjustments, proper hydration, and monitoring autonomic metrics-offers the most holistic pathway to improvement!!! Let's keep sharing successes and protocols!!!
August 8, 2023 at 18:30