When you take a pill, the active pharmaceutical ingredient, the biologically active component that produces the therapeutic effect in a medication. Also known as API, it’s the reason the drug works — whether it’s lowering blood pressure, killing bacteria, or blocking pain signals. But behind every pill is a hidden challenge: making sure enough of this ingredient is always available. That’s where an API reserve, a strategic stockpile of active pharmaceutical ingredients held by manufacturers or governments to prevent shortages comes in. Without it, even the most effective medicine can disappear from shelves — not because no one makes it, but because the raw material ran out.
API reserves aren’t just about keeping drugs in stock. They’re about controlling risk. Many APIs are made in just one or two factories overseas, often in India or China. If a factory shuts down for inspection, a natural disaster hits, or trade rules change, the whole supply chain can freeze. That’s why major drugmakers and health agencies build reserves — sometimes months’ worth — of critical APIs like those used in antibiotics, heart meds, and cancer treatments. The drug supply chain, the network of manufacturers, distributors, and regulators that move active ingredients from labs to patients depends on these buffers. When reserves are low, generic drug makers delay launches — even if their pills are FDA-approved — because they can’t get the core ingredient. You’ve seen this in action: shortages of metformin, levothyroxine, or even basic antibiotics. It’s not a glitch. It’s a system under pressure.
Building an API reserve isn’t simple. It costs money. It needs secure storage. It requires tracking expiration dates and managing quality control over time. Some countries now require drugmakers to report their API inventory levels. Others are investing in domestic production to reduce foreign dependence. But even with all this, reserves are often too small, too fragmented, or too hidden from public view. The result? Patients wait. Doctors prescribe alternatives. Pharmacists scramble. And behind it all is a single, invisible molecule — the API — that holds everything together. Below, you’ll find real stories and data on how API shortages impact treatment, why generic drug approvals stall, how manufacturers track these ingredients, and what’s being done to fix the gaps. These aren’t abstract policies. They’re the reason your prescription might be late — or unavailable.
Posted by
Paul Fletcher
8 Comments
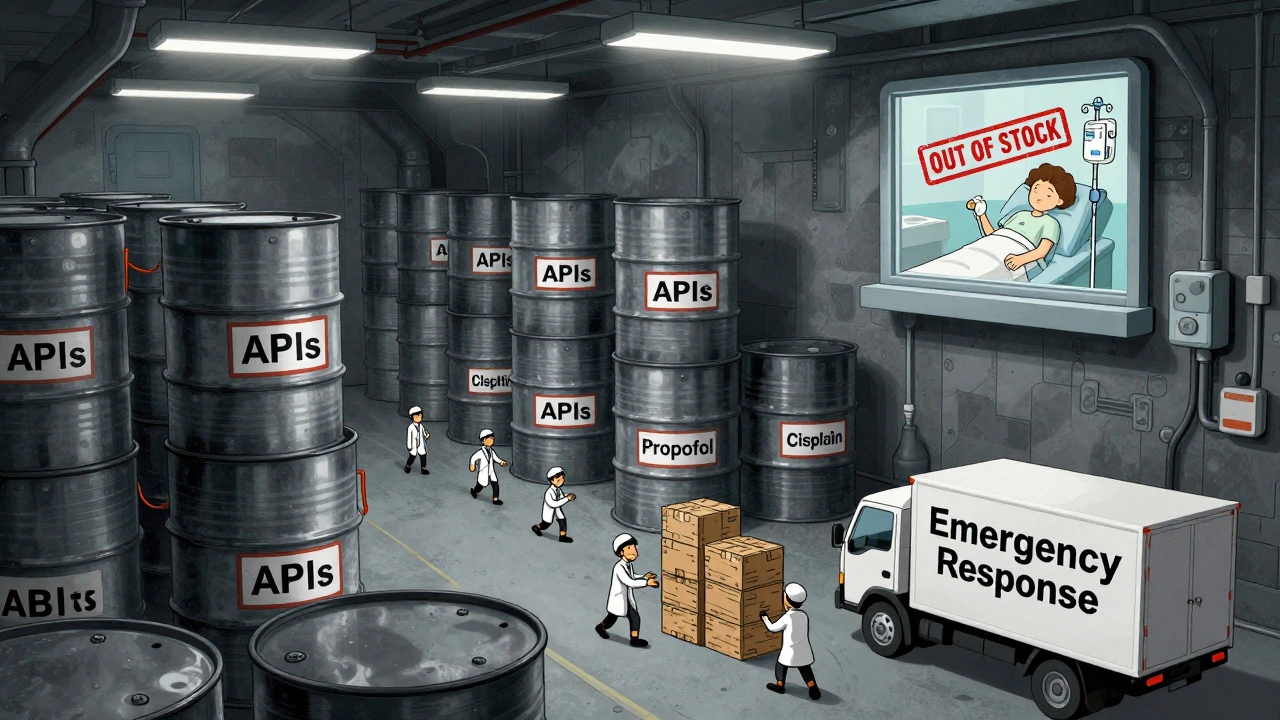
In 2025, the U.S. government expanded its drug shortage response with a new API stockpile program, but gaps in enforcement, funding, and economic incentives leave hospitals and patients vulnerable to ongoing shortages of critical medications.
read more