When a drug you rely on suddenly isn’t available, it’s not just an inconvenience—it’s a health risk. Drug shortages, the sudden lack of essential medications in the supply chain. Also known as medication unavailability, they happen when manufacturers can’t produce enough, regulators delay approvals, or economic pressures make production unprofitable. This isn’t rare. In 2023 alone, over 300 drugs faced shortages in the U.S., including antibiotics, cancer treatments, and even basic pain relievers. These gaps don’t just delay care—they force doctors to switch patients to less effective, more expensive, or riskier alternatives.
Behind every shortage is a chain of problems. Generic drug delays, when FDA-approved medications sit on shelves because of legal battles or manufacturing issues, are a major driver. A drug might pass science tests but get stuck in patent lawsuits or quality inspections. FDA approval, the process that ensures drugs are safe and effective before reaching patients, isn’t the finish line—it’s just the start. Even after approval, companies may stop making a drug if it’s too cheap to profit from, especially when bulk orders go to the lowest bidder. And when one factory has a problem—contamination, equipment failure, staffing issues—the whole supply can collapse.
These aren’t abstract policy issues. They hit real people. A cancer patient waiting for a chemotherapy drug. A diabetic running out of insulin. A parent whose child needs an antibiotic that’s been pulled from shelves. Medication access, how easily patients can get the drugs they need, when they need them is breaking down. Some pharmacies ration doses. Others switch to pricier brands. Patients skip doses or go without. And while online pharmacies and home delivery services try to fill gaps, they can’t create drugs that don’t exist.
What’s being done? The FDA tracks shortages and tries to speed up approvals. Some states are building emergency stockpiles. Pharmacies are working with manufacturers to find alternatives. But the system still relies on a fragile network of global suppliers, thin profit margins, and slow regulatory responses. The real fix? More transparency, better incentives for manufacturers, and policies that treat essential medicines like public infrastructure—not just commodities.
Below, you’ll find real stories and data-backed insights into why these shortages happen, how they’re being managed, and what you can do if your medication disappears. From how the FDA monitors generics after approval to why biosimilars struggle to enter the market, these articles show the hidden forces behind your prescription bottle.
Posted by
Paul Fletcher
8 Comments
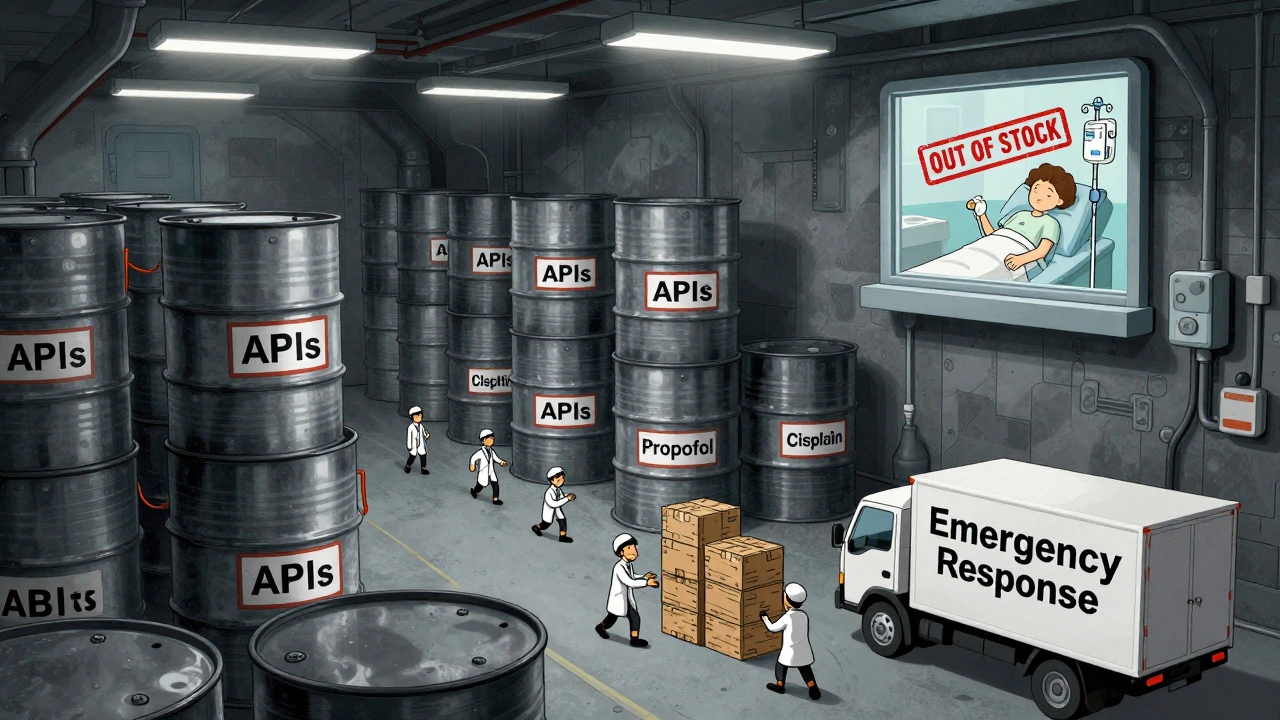
In 2025, the U.S. government expanded its drug shortage response with a new API stockpile program, but gaps in enforcement, funding, and economic incentives leave hospitals and patients vulnerable to ongoing shortages of critical medications.
read more