When the FDA drug shortages, occurrences where essential medications are unavailable in the U.S. market due to manufacturing, regulatory, or economic issues. Also known as pharmaceutical supply gaps, these disruptions don’t just cause inconvenience—they can delay cancer treatments, worsen chronic conditions, and force patients onto riskier alternatives. This isn’t rare. In 2023 alone, over 300 drugs hit shortage lists, including antibiotics, chemotherapy agents, and even basic IV fluids. Many of these aren’t brand-name drugs. They’re the cheap generics you rely on—because they’re supposed to be easy to make, cheap to produce, and always in stock.
But here’s the problem: making a generic drug isn’t just about copying a pill. It requires FDA approval, sterile facilities, approved raw materials, and consistent quality control. A single factory failure—like a contaminated batch or an unannounced inspection—can halt production for months. And when one plant makes 80% of a drug, like many do, that’s not just a hiccup. It’s a crisis. generic drug supply, the network of manufacturers and distributors that provide affordable versions of branded medications is fragile. It’s built on thin margins, global sourcing, and just-in-time inventory. No one plans for a shortage because no one profits from stocking extra.
That’s why medication access, a patient’s ability to obtain prescribed drugs without delays or financial barriers is tied directly to these shortages. If your doctor prescribes a generic diuretic for high blood pressure, but it’s unavailable, you might get switched to a more expensive brand—or worse, go without. Patients with cancer, epilepsy, or heart failure don’t get to wait. And when pharmacies run out, they turn to other suppliers, sometimes with unknown quality. The drug supply chain, the complex system linking raw material suppliers, manufacturers, distributors, and pharmacies has too many weak links. One broken connection can ripple across the country.
The FDA tracks these shortages and tries to warn providers, but they can’t force companies to make more. They can’t fix a factory. They can’t pay for more raw materials. And they can’t override patents or economic decisions that make some drugs unprofitable to produce. Meanwhile, patients are left guessing: Is my med gone for a week? A month? Forever? Some shortages last years. Some drugs never come back.
What you’ll find below are real stories from people affected by these gaps—and the deep dives into why they happen. From how tentative approvals sit on shelves for years, to how post-market monitoring catches safety issues that delay production, to how insurers and specialty pharmacies navigate the chaos. You’ll learn which drugs are most at risk, how to spot a shortage before it hits your pharmacy, and what you can do to protect your treatment plan. This isn’t theory. It’s what’s happening right now, to real people, every single day.
Posted by
Paul Fletcher
8 Comments
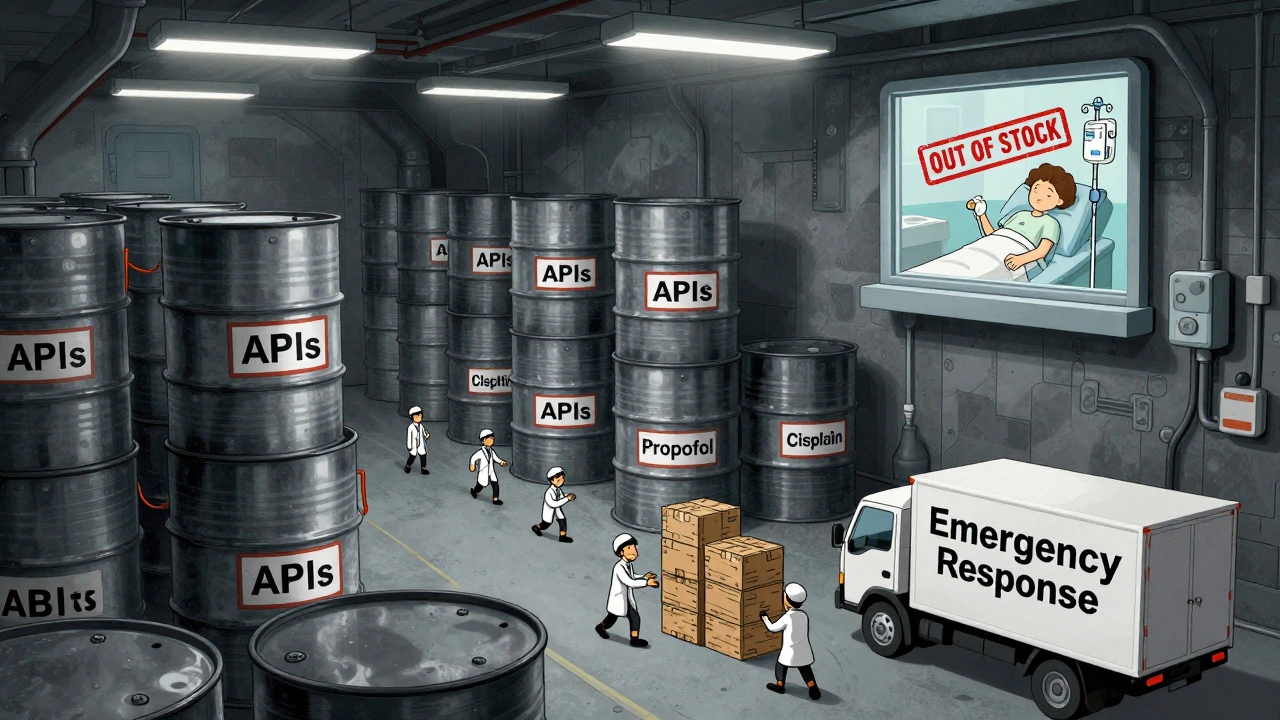
In 2025, the U.S. government expanded its drug shortage response with a new API stockpile program, but gaps in enforcement, funding, and economic incentives leave hospitals and patients vulnerable to ongoing shortages of critical medications.
read more