When you think about how your prescription gets to the pharmacy, you might picture a doctor’s note and a trip to the counter. But behind that simple step is a complex government drug supply, a network of public agencies, manufacturers, and distributors that ensure essential medicines reach patients, especially those who can’t afford them. Also known as public pharmaceutical distribution, this system includes everything from bulk purchasing by Medicare to emergency stockpiles for outbreaks—and it’s far from perfect. In the U.S., agencies like the FDA, CDC, and HHS work with state health departments to manage drug availability, but funding gaps, patent battles, and manufacturing delays mean many people wait weeks—or never get their meds at all.
The generic drug, a lower-cost version of a brand-name medicine that meets the same safety and effectiveness standards. Also known as off-patent drugs, it is the backbone of the government drug supply. Over 90% of prescriptions filled in America are generics, and public programs like Medicaid rely on them to keep costs down. But here’s the catch: just because a drug is approved doesn’t mean it’s available. The FDA gives tentative approval, a green light for generics that can’t yet be sold due to legal or patent issues. Also known as pre-market clearance, this status often sits for years while lawsuits drag on. That’s why some life-saving generics—like those for cancer or epilepsy—never make it to shelves, even though they’re scientifically ready. Meanwhile, the FDA approval, the official authorization for a drug to be sold in the U.S. after proving safety and efficacy. Also known as market authorization, this process is only the start—post-market monitoring through systems like FAERS tracks side effects long after launch, catching problems clinical trials miss.
Access isn’t just about supply—it’s about equity. A child with hemophilia, a cancer patient on oral chemo, or an elderly person on insulin all depend on consistent drug availability. When the government drug supply falters, it’s not just a policy issue—it’s a health crisis. That’s why posts here dig into why some generics never reach patients, how insurers shape what’s available through formularies, and how specialty pharmacies manage complex drugs like biosimilars. You’ll also find real stories behind the numbers: how smoking affects clozapine levels, why missed doses lead to resistance, and how delivery services are filling gaps left by broken systems. This isn’t theory. It’s what’s happening right now—and what you need to know to get the care you’re entitled to.
Posted by
Paul Fletcher
8 Comments
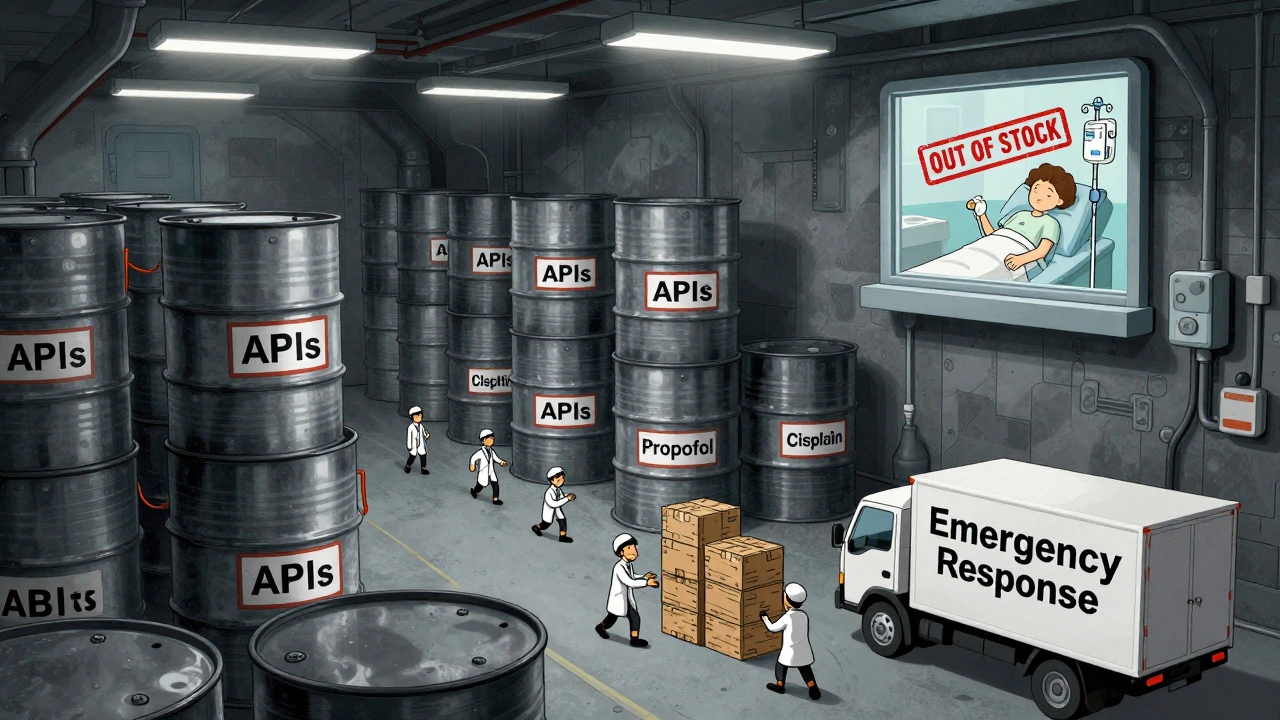
In 2025, the U.S. government expanded its drug shortage response with a new API stockpile program, but gaps in enforcement, funding, and economic incentives leave hospitals and patients vulnerable to ongoing shortages of critical medications.
read more