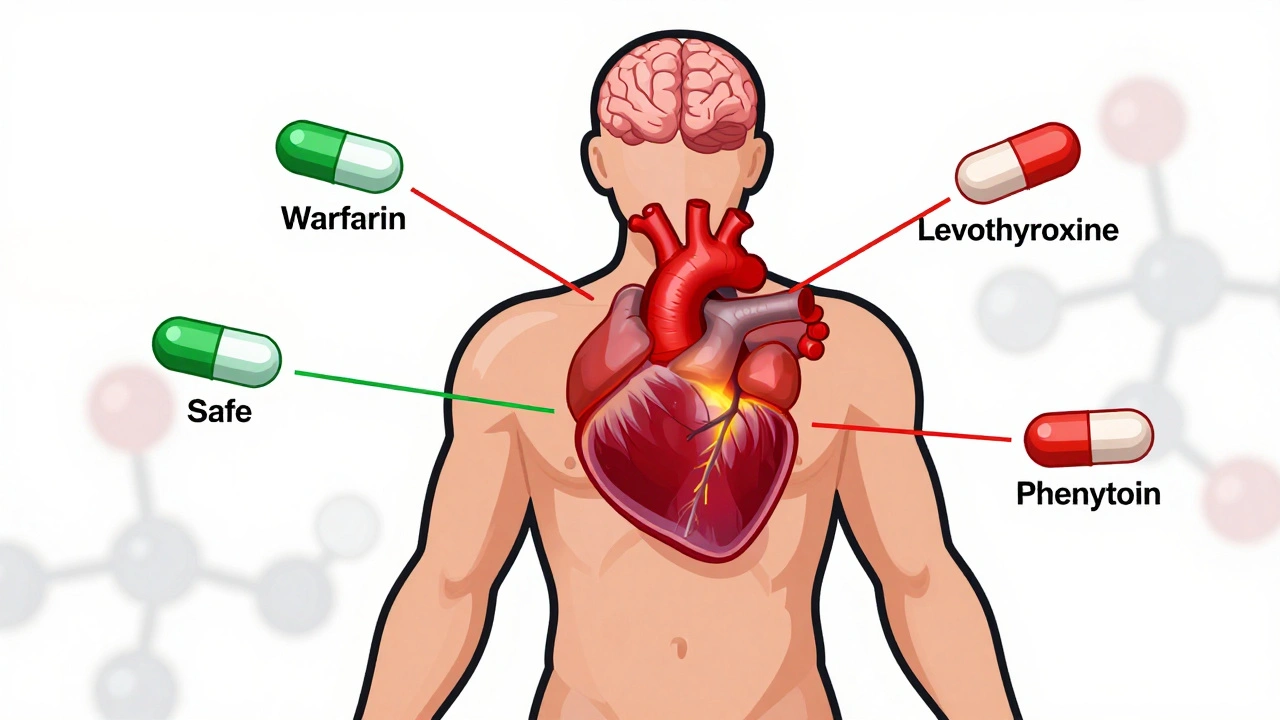
When you hear NTI generics, generic versions of drugs with a narrow therapeutic index, meaning small changes in dose can lead to serious side effects or treatment failure. Also known as narrow therapeutic index drugs, these medications require precision—whether brand or generic—because the difference between working and causing harm is tiny. Think of them like a scalpel instead of a hammer. One wrong move, and things go wrong fast. Drugs like warfarin, levothyroxine, phenytoin, and cyclosporine fall into this category. They’re not just any pills. They’re the ones your doctor watches closely, the ones where even a 10% difference in absorption can mean a seizure, a blood clot, or organ rejection.
That’s why the FDA treats NTI generics, generic versions of drugs with a narrow therapeutic index, meaning small changes in dose can lead to serious side effects or treatment failure. Also known as narrow therapeutic index drugs, these medications require precision—whether brand or generic—because the difference between working and causing harm is tiny. differently. Most generics just need to match the brand’s average performance. But for NTI drugs, the FDA demands tighter bioequivalence standards—often requiring the generic to deliver the same amount of drug within a much smaller range. This isn’t just bureaucracy. It’s safety. A 2023 study in Pharmacoepidemiology & Drug Safety found that patients switched from brand to generic NTI drugs had a 23% higher chance of hospitalization in the first 90 days if the generic wasn’t properly validated. Not because generics are bad, but because some weren’t built to handle the precision these drugs demand.
That’s where tentative FDA approval, a status given to generic drugs that are scientifically ready but blocked by patents or legal issues from hitting the market. Also known as ANDA tentative approval, this status means the drug meets all technical standards—but still can’t be sold yet. comes in. Many NTI generics sit in this limbo. They’re proven to work, but legal battles or patent extensions keep them off shelves. Meanwhile, patients pay more for the brand, even when a safer, cheaper generic could be available. And even when they do launch, not all NTI generics are created equal. Some manufacturers cut corners on fillers, coatings, or dissolution rates—details that don’t show up in basic lab tests but can change how the drug behaves in your body.
That’s why post-marketing pharmacovigilance, the ongoing monitoring of drug safety after approval using real-world data, patient reports, and inspections. Also known as drug surveillance, this process catches problems clinical trials miss. matters so much for NTI generics. The FDA doesn’t just approve them and walk away. They track adverse events through FAERS, inspect manufacturing sites, and analyze pharmacy claims. If a generic version of levothyroxine starts showing up in reports of unexplained heart palpitations or weight swings, they investigate. Fast. Because with NTI drugs, one bad batch can hurt dozens—or hundreds—of people.
You might wonder: why not just stick with the brand? Cost. A brand-name NTI drug can cost $300 a month. The generic? Often under $20. But that savings means nothing if the switch makes you sick. That’s why talking to your doctor about generic vs brand-name medications, the choice between lower-cost generic drugs and their more expensive branded counterparts. Also known as brand vs generic drugs, this decision affects both your wallet and your health. isn’t just about money—it’s about control. Ask if your prescription is an NTI drug. Ask if the generic you’re getting has been tested for tight bioequivalence. Ask if your pharmacy is switching brands behind your back. You have the right to know. And in some cases, you have the right to refuse a switch.
Below, you’ll find real stories and data from patients, doctors, and regulators. You’ll see how NTI generics are monitored, why some never reach shelves, how insurers handle them, and what you can do to protect yourself when switching meds. No fluff. No marketing. Just what you need to know to make sure your next prescription doesn’t just save money—it saves your health.
Posted by
Paul Fletcher
8 Comments
NTI generics require stricter regulation than standard generics due to narrow margins between effective and toxic doses. This article explores how the FDA, EMA, Canada, and Japan differ in their approaches, what’s changing in 2025, and why prescribers must stay cautious.
read more