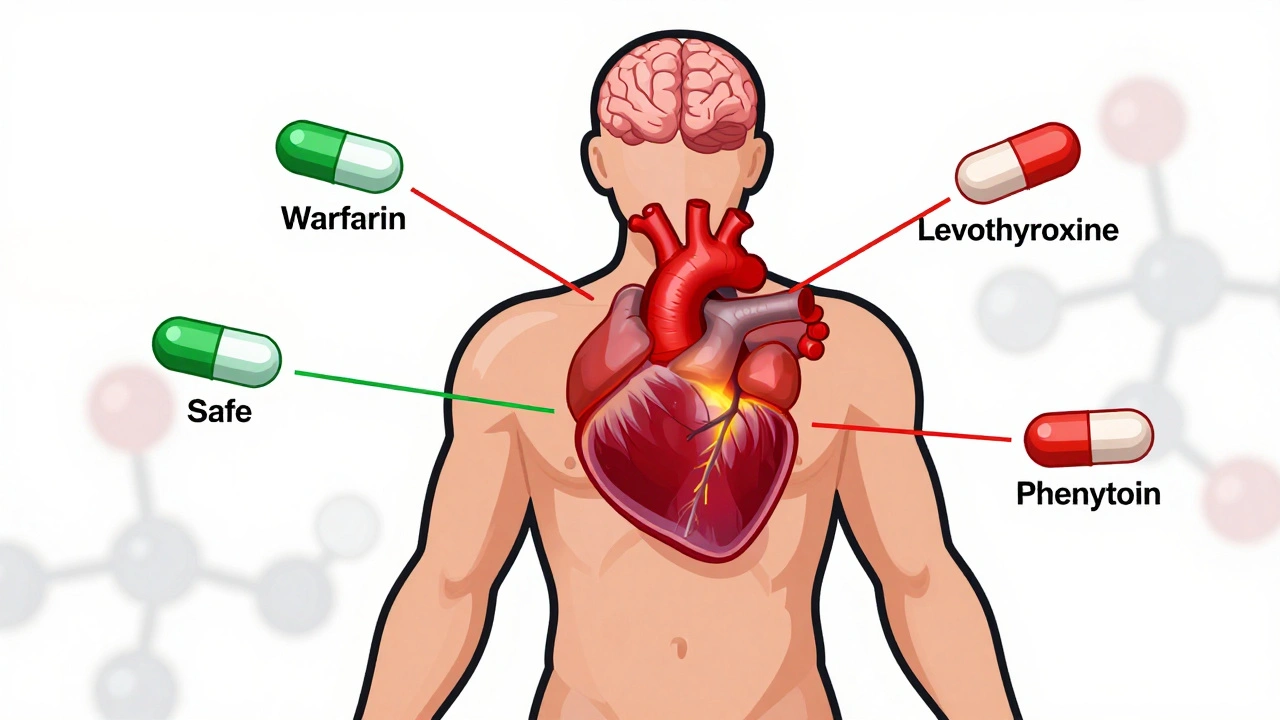
When a drug has a narrow therapeutic index, the range between an effective dose and a toxic one is very small. Also known as a narrow therapeutic window, this means even a slight mistake in dosage can lead to serious harm—or make the drug useless. You won’t find this label on most pills, but if you’re taking warfarin, lithium, digoxin, or cyclosporine, you’re already dealing with one.
These drugs don’t give you room for error. Take too little, and the condition doesn’t improve. Take too much, and you risk organ damage, seizures, or even death. That’s why doctors often order therapeutic drug monitoring, regular blood tests to measure how much of the drug is in your system. It’s not about guessing—it’s about knowing exactly what’s in your bloodstream. This isn’t optional for these medications; it’s standard practice. And it’s why switching from a brand to a generic version can be risky if the formulation isn’t bioequivalent down to the last milligram. The FDA requires generics to match the brand, but even small differences in absorption can push a drug with a narrow therapeutic index into dangerous territory.
These drugs also react strongly to other things in your life. Smoking, for example, can change how fast your body breaks down clozapine, a drug with a narrow therapeutic index. Eating grapefruit might interfere with your statin. Skipping a dose or taking it with food when you’re supposed to take it on an empty stomach? That’s not just inconvenient—it can be life-threatening. That’s why medication adherence, taking your drug exactly as prescribed isn’t just a buzzword here—it’s survival. And why pharmacovigilance systems track real-world side effects so closely for these medications. One patient’s reaction can reveal a pattern that clinical trials never caught.
If you’re on a drug with a narrow therapeutic index, you’re not just a patient—you’re a partner in your own safety. You need to know the name of your drug, why it’s different from others, and what signs mean trouble. That’s why understanding how your body responds to it matters more than ever. The posts below cover exactly these kinds of high-stakes scenarios: how drug interactions change levels, why generic substitutions require caution, how monitoring works in practice, and what happens when things go wrong. These aren’t theoretical discussions. They’re real-world guides for people who can’t afford a single mistake.
Posted by
Paul Fletcher
15 Comments

Track your body's response when switching to generic medications with a simple medication journal. Learn what to record, when it matters most, and how to use your notes to get better care.
read morePosted by
Paul Fletcher
8 Comments
NTI generics require stricter regulation than standard generics due to narrow margins between effective and toxic doses. This article explores how the FDA, EMA, Canada, and Japan differ in their approaches, what’s changing in 2025, and why prescribers must stay cautious.
read more